Scroll to:
Views of traditional healers on collaboration with health professionals when managing epilepsy in rural areas of Limpopo and Mpumalanga Provinces (South Africa)
https://doi.org/10.17749/2077-8333/epi.par.con.2023.165
Abstract
Objective: to explore traditional healers’ views on epilepsy management in collaboration with health professionals in South Africa rural communities.
Material and methods. A qualitative research approach using explorative, descriptive and contextual designs was adopted for the study in Limpopo and Mpumalanga Provinces. Non-probability, snowball purposive sampling was used to sample 20 traditional healers. Data were collected through in-depth individual interviews at the participants’ homes and analysed using Tesch's eight steps of open coding data analysis.
Results. Findings revealed two themes, namely: a perspective on collaboration in epilepsy treatment and strategies to enhance its implementation. Most traditional healers were unaware of the official collaboration in managing epilepsy. When they found out about it, most of them were willing to collaborate with health professionals.
Conclusion. There is a need to strengthen mutual respect, open dialogue, mutual referral and capacity building to achieve collaboration in managing epilepsy effectively.
For citations:
Nemathaga M., Maputle M.S., Makhado L., Mashau N.S. Views of traditional healers on collaboration with health professionals when managing epilepsy in rural areas of Limpopo and Mpumalanga Provinces (South Africa). Epilepsy and paroxysmal conditions. 2023;15(3):222–231. https://doi.org/10.17749/2077-8333/epi.par.con.2023.165
INTRODUCTION / ВВЕДЕНИЕ
Epilepsy is a chronic neurological condition affecting around 50 million people worldwide, with the highest prevalence in low-income countries, particularly sub-Saharan Africa, as reported by F. Boumediene et al. [1] and the World Health Organization (WHO) [2]. It is characterized by recurring seizures, which can involve either a small part of the body (partial) or the entire body (generalized) and may be accompanied by loss of consciousness and control over bowel or bladder function. Sadly, 75% of individuals with epilepsy in low-income countries do not receive the necessary treatment. In the Indian subcontinent, traditional healers are often the primary healthcare providers, and people who believe that supernatural forces cause epilepsy tend to seek their services. As a result, anti-epileptic treatment is often delayed, and many individuals in the community remain untreated [3].
According to S. Kwedi Nolna et al. [4], in sub-Saharan Africa, most of the population (85%) seek the help of traditional healers to diagnose and treat their illnesses. The World Health Organization recognizes the vital role that traditional medicine plays in healthcare and suggests that traditional healers should be integrated into the healthcare system. These healers use a culturally sensitive approach and are respected members of their community, as E. Krah et al. [5] noted. Rural residents find traditional medicine appealing as it is more accessible and cost-effective than the existing healthcare system [5]. R.M. Siriba1 conducted a study in Limpopo province, revealing that cultural beliefs significantly impact the healthcare-seeking behaviors of people living with epilepsy (PLWE) and their families.
Consequently, these cultural factors often lead individuals to consult traditional healers instead of Western-trained healthcare professionals. This delay in seeking a proper diagnosis and treatment compromises the quality of life of PLWE and their families. However, a recent study conducted in South Africa found that both traditional healers and healthcare practitioners recognized the benefits of collaboration, which could provide more culturally appropriate treatment for PLWE [6]. The traditional healers are often (sociocultural) acceptable and able to explain conditions drawing on locally relevant terms.
Traditional healers and healthcare professionals have coexisted within the healthcare system for many years. However, in most health policies worldwide, healthcare professionals are recognized as the official providers of healthcare [7]. The WHO emphasizes the importance of collaboration between traditional healers and healthcare professionals, particularly regarding the management of epilepsy, as traditional healers can significantly influence the health-seeking behaviour of PLWE. Collaboration between traditional and biomedical medicine can lead to holistic care and improved health outcomes for people with chronic conditions [8]. Nevertheless, there is a limited evidence-based collaborative relationship between traditional healers and healthcare professionals in rural communities in South Africa.
Objective: to explore traditional healers’ views on epilepsy management in collaboration with health professionals in rural communities of Limpopo and Mpumalanga Provinces.
MATERIAL AND METHODS / МАТЕРИАЛ И МЕТОДЫ
The research was conducted in rural communities located in Limpopo (Fig. 1) and Mpumalanga (Fig. 2).
In Limpopo, the selected communities were Malavuwe, Mtititi, and Bochum, while in Mpumalanga, the communities selected were Clara, Acornhoek, and Jerusalem. These communities are diverse, with different cultural beliefs and practices. The selection of these communities was based on their cultural beliefs and practices, on the management of epilepsy. Previous research indicates that people living with epilepsy in these villages tend to seek the services of traditional healers as their first line of treatment, which can delay access to proper medical treatment for epilepsy.
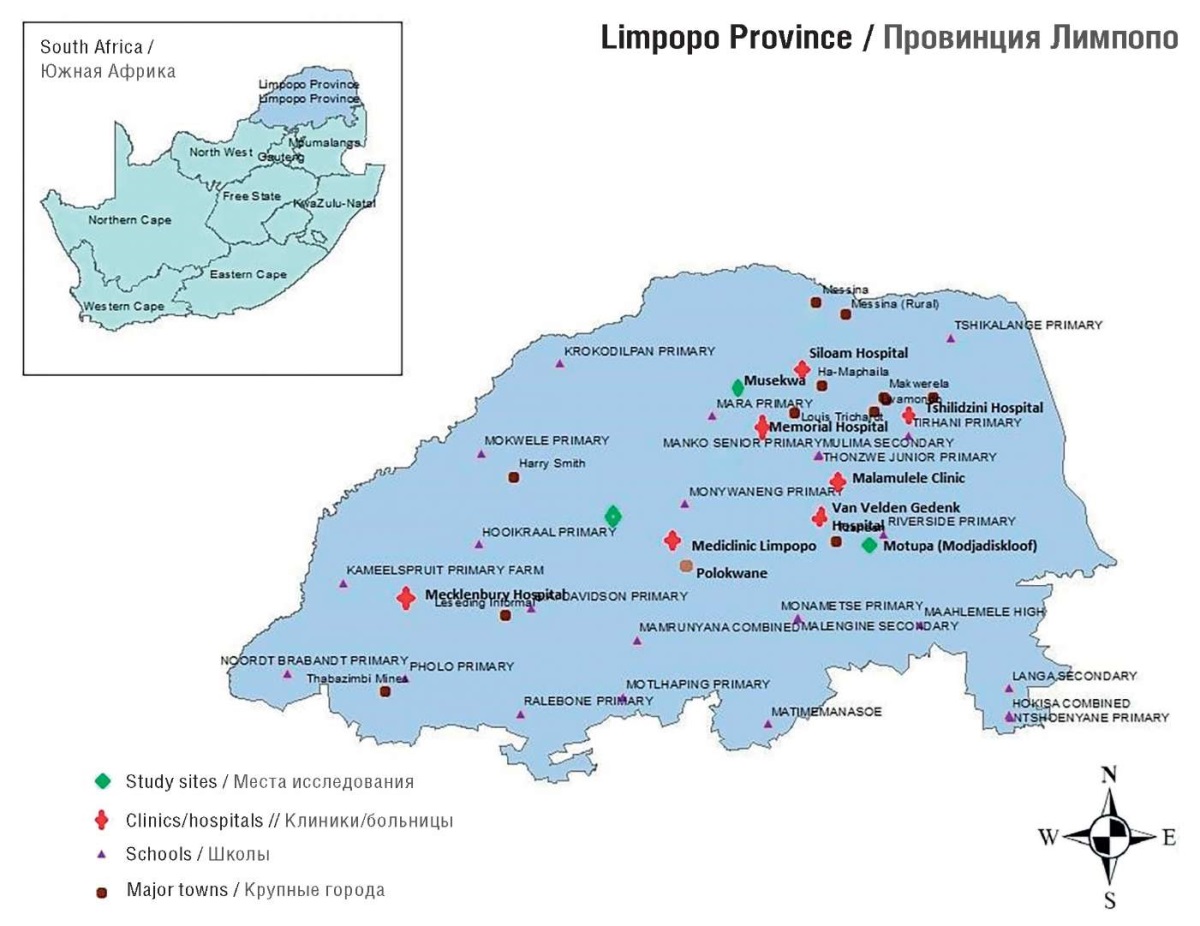
Figure 1. Limpopo Province map (South Africa)
Рисунок 1. Карта провинции Лимпопо (Южная Африка)
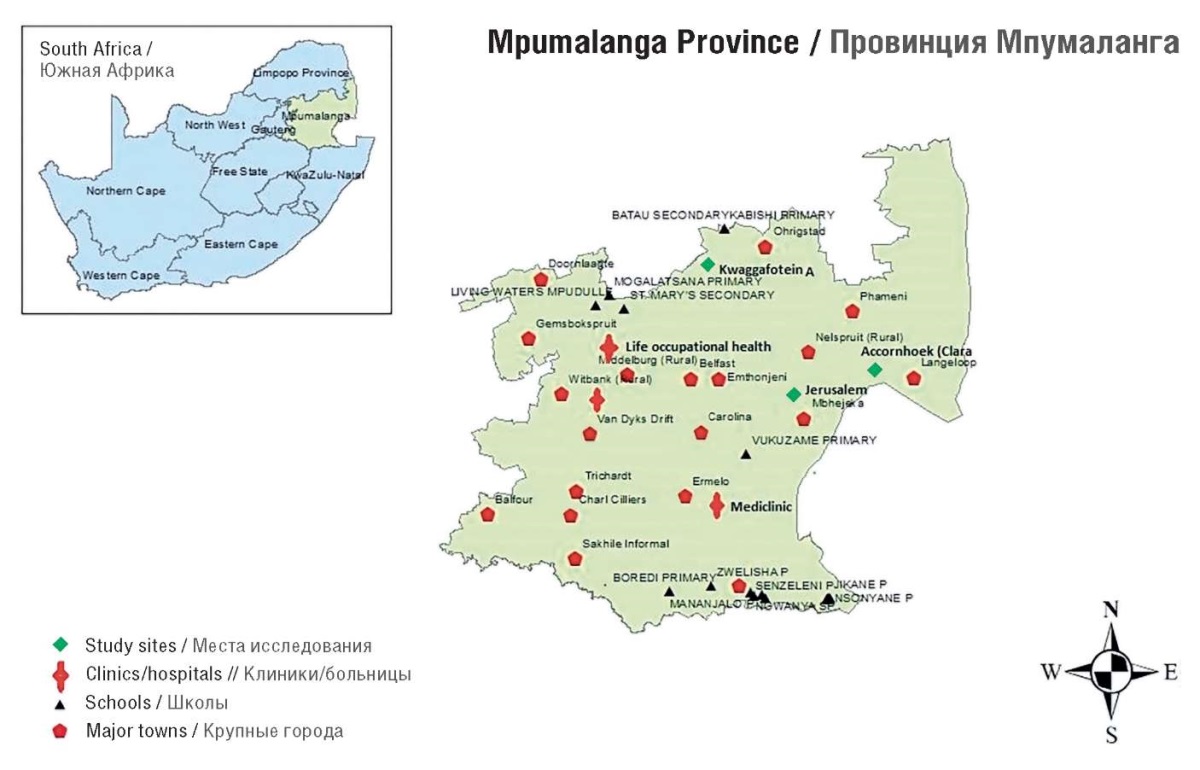
Figure 2. Mpumalanga Province map (South Africa)
Рисунок 2. Карта провинции Мпумаланга (Южная Африка)
Design / Дизайн
An explorative, descriptive, and contextual research design using a qualitative approach was employed. Researchers directly engaged with the participants to obtain detailed and comprehensive data [9].
Population and sampling / Популяция и выборка
The study involved traditional healers responsible for managing epilepsy in the selected rural communities of Limpopo and Mpumalanga provinces. The villages were sampled based on their cultural diversity using purposive sampling. Snowball sampling [9]. was also utilized to select traditional healers, where one identified traditional healer and referred the researchers to other traditional healers who manage epilepsy. The sample consisted of 20 traditional healers providing epilepsy care in the selected rural communities. Only traditional healers with the responsibility of managing epilepsy were included in the study.
Measures to ensure trustworthiness / Меры по обеспечению достоверности
Credibility, transferability, dependability, and confirmability were used to assure trustworthiness [10]. Credibility was ensured through prolonged engagement and member checks. A thorough explanation of the research methodology and the findings were provided. Additionally, the individuals' backgrounds were extensively described to ensure transferability [9]. The methods of this study were described in detail so that future researchers might replicate the work, if not necessarily to obtain the same results, to address the dependability criteria more directly. To allow the integrity of research findings to be scrutinized, in-depth methodological description was done [11].
Pre-test of the interview questions / Предварительная проверка вопросов
The researchers selected two participants from rural Limpopo and Mpumalanga Provinces to pre-test the questions before data collection [12]. The selected participants were interviewed to check whether the question was phrased in a manner they understood, and this data was not included in the main study. The purpose of pre-test was to determine whether the question was presented in a way that the selected participants could understand. Interviews were conducted to check clarity. The duration of the pre-test was 35 to 40 minutes.
Ethical considerations / Этические аспекты
The researchers complied with the requirements of the Helsinki Declaration of the World Medical Association (Fortaleza, Brazil, 2013). They conform to generally accepted scientific principles, that were based on a thorough knowledge of the scientific literature, other relevant sources of information. Ethical clearance was obtained from the University of Venda Human and Clinical Trial Research Ethics Committee (SHS/19/PH/37/2101). Permission to access the villages was received from the Traditional Councils and participants. Participation was voluntary, and they were informed of the right to abstain from participation or to withdraw consent to participate at any time without reprisal. Researchers adhered to ethical principles of respect for persons, informed consent, privacy, confidentiality and anonymity.
Data collection / Сбор данных
Data collection was done through in-depth individual interviews at the participants’ homes. The duration of the interviews was 40 to 45 minutes. The interviews were conducted in the native language (Sepedi, Xitsonga and Tshivenda). The following central question guided the interviews: “Kindly share your views on collaboration of traditional healers with health professionals when managing epilepsy?” A voice recorder was used after obtaining consent from participants.
In order for the participants to provide more clarity, probing questions were posed emanating from their responses. Furthermore, techniques like listening, clarifying, reflecting, focusing, and paraphrasing were used. A free flow of information and an encouragement to talk was made possible by minimal verbal responses like nodding the head, saying “mm,” “Yes,” and “continue.” Because of this, participants were more at ease and willing to talk about their management [12].
Data analysis / Анализ данных
To analyse data, this study adopted Tesch's open coding data analysis guide [13]. Tesch’s lists eight procedures to consider when analysing qualitative data.
The researchers listened to the voice recorder and transcribed it verbatim. Thereafter, researchers read through one transcript at a time to obtain a good picture of the participant’s responses. Related data were written and categorised together. Sub-themes were formed, which were then clustered into columns. Following that, a list of themes was created for each topic. Columns were created by grouping similar clusters together. Multiple coloured pens were used to facilitate the process. The subjects were after that coded and written next to the appropriate segments by the researchers. The researchers used tables to display the analysis findings. The tables were arranged based on the researchers’ themes and sub-themes.
Data sharing statement / Заявление о предоставлении данных
The raw data used to support the findings of this study are included in the article and can be available from the corresponding author upon request.
RESULTS / РЕЗУЛЬТАТЫ
Demographic profile / Демографический профиль
The population comprised participants, including males (n=9) and females (n=11). The age of participants ranged between 35 and 62 years. Most participants (n=11) were from Limpopo, and the rest (n=9) were from Mpumalanga Province. All male participants (n=9) were married and trained for traditional healing. Only a few (n=4) females were married and qualified. The remaining female participants (n=7) were not married. Tshivenda was the most common language spoken, followed by Xitsonga and Sepedi. Table 1 illustrates the demographic profile of participants.
Two themes emerged from the findings: a perspective on collaboration in epilepsy treatment and strategies to enhance the implementation of collaboration (Table 2).
Table 1. Demographic profile of study participants
Таблица 1. Демографические характеристики участников исследования
|
Participant / Участник |
Gender/ Пол |
Marital status / Семейное положение |
Highest grade passed / Образование |
Age, years / Возраст, лет |
Year started practicing / Год начала практики |
Trained as traditional healer / Подготовка в качестве традиционного целителя |
|
Participant 1 / Участник 1 |
Male / Мужской |
Married / Женат |
Grade 8 / 8 классов |
60 |
2003 |
No / Нет |
|
Participant 2 / Участник 2 |
Female / Женский |
Married / Замужем |
Grade 12 / 12 классов |
56 |
1998 |
Yes / Да |
|
Participant 3 / Участник 3 |
Male / |
Married / Женат |
Grade 3 / 3 класса |
54 |
2006 |
No / Нет |
|
Participant 4 / Участник 4 |
Female / Женский |
Married / Замужем |
Grade 5 / 5 классов |
56 |
2001 |
Yes / Да |
|
Participant 5 / Участник 5 |
Male / Мужской |
Married / Женат |
Grade 5 / 5 классов |
55 |
2006 |
Yes / Да |
|
Participant 6 / Участник 6 |
Male / Мужской |
Married / Женат |
Grade 11 / 11 классов |
52 |
1998 |
Yes / Да |
|
Participant 7 / Участник 7 |
Female / Женский |
Single / Не замужем |
Grade 8 / 8 классов |
60 |
2011 |
Yes / Да |
|
Participant 8 / Участник 8 |
Female / Женский |
Single / Не замужем |
Grade 6 / 6 классов |
58 |
2002 |
Yes / Да |
|
Participant 9 / Участник 9 |
Female / Женский |
Single / Не замужем |
Grade 12 / 12 классов |
35 |
2011 |
Yes / Да |
|
Participant 10 / Участник 10 |
Male / Мужской |
Married / Женат |
Grade 3 / 3 класса |
50 |
2008 |
Yes / Да |
|
Participant 11 / Участник 11 |
Male / Мужской |
Married / Женат |
Grade 10 / 10 классов |
60 |
2010 |
No / Нет |
|
Participant 12 / Участник 12 |
Female / Женский |
Married / Замужем |
Grade 8 / 8 классов |
51 |
2012 |
Yes / Да |
|
Participant 13 / Участник 13 |
Female / Женский |
Single / Не замужем |
Grade 3 / 3 класса |
36 |
2007 |
No / Нет |
|
Participant 14 / Участник 14 |
Female / Женский |
Married / Замужем |
Grade 12 / 12 классов |
38 |
2014 |
Yes / Да |
|
Participant 15 / Участник 15 |
Female / Женский |
Single / Не замужем |
Grade 6 / 6 классов |
47 |
2001 |
Yes / Да |
|
Participant 16 / Участник 16 |
Female / Женский |
Married / Замужем |
Grade 4 / 4 класса |
62 |
2012 |
Yes / Да |
|
Participant 17 / Участник 17 |
Male / Мужской |
Married / Женат |
Grade 12 / 12 классов |
59 |
2004 |
No / Нет |
|
Participant 18 / Участник 18 |
Male / Мужской |
Married / Женат |
Grade 3 / 3 класса |
51 |
1999 |
No / Нет |
|
Participant 19 / Участник 19 |
Female / Женский |
Single / Не замужем |
Grade 9 / 9 классов |
38 |
2002 |
Yes / Да |
|
Participant 20 / Участник 20 |
Male / Мужской |
Married / Женат |
Degree / Высшее |
54 |
2005 |
Yes / Да |
Table 2. Study themes and sub-themes
Таблица 2. Темы и подтемы исследования
|
Theme / Тема |
Sub-theme / Подтема |
||
|
1 |
A perspective on collaboration in epilepsy treatment / Взгляд на сотрудничество при лечении эпилепсии |
1.1
|
Positive perspective on collaboration when treating epilepsy / Положительный взгляд на сотрудничество при лечении эпилепсии |
|
1.2 |
Negative perspective on collaboration when treating epilepsy / Отрицательный взгляд на сотрудничество при лечении эпилепсии |
||
|
2 |
Strategy to enhance the implementation of collaboration / Стратегия по улучшению реализации сотрудничества |
2.1
|
Mutual referral system / Система перенаправления больных |
|
2.2 |
Creation of opportunities for consultation rooms accessibility within the health facility / Создание консультационных кабинетов в лечебных учреждениях |
||
Theme 1. A perspective on collaboration in epilepsy treatment / Тема 1. Взгляд на сотрудничество при лечении эпилепсии
This study findings revealed that most traditional healers are willing to collaborate with health professionals. They were unaware of the official collaboration that was said to exist in managing epilepsy between traditional healers and healthcare professionals. The traditional healers mentioned working together on the Safe Motherhood Programme, National Tuberculosis Programme, and National HIV/AIDS Prevention Programme. However, few of them disagree entirely with collaboration because they believe that they manage epilepsy in a different way and spiritual epilepsy cannot be managed or treated medically. Two sub-themes emerged from the findings as discussed below.
Sub-theme 1.1. Positive perspective on collaboration when treating epilepsy
Collaboration with health professionals was acknow-ledged as the best strategy to promote early diagnosis and treatment of epilepsy by most traditional healers. The following quotes supported the findings:
“I would like to work with health care professionals as long as they understand that some diseases cannot be cured medically. For instance, if the epilepsy was caused by witchcraft, then traditional healing is required” (Female, 38 years old).
“The Government needs to recognise us and allocate us in hospitals so that we can assist doctors in diagnosing and treating epilepsy. We are very knowledgeable and skilled” (Male, 59 years old).
“I would work with health professionals, I don’t have any problem. If we have to negotiate a consultation fee, I would gladly refer the clients if necessary. There must be an agreement, I can’t share my knowledge and work free of charge” (Male, 54 years old).
“Working with health professionals would improve the management of epilepsy because I will treat the clients with traditional medicines, and doctors will treat epilepsy using Western medicines. There won’t be any confusion about the treatment choice because we will work together’’ (Female, 62 years old).
Participants had positive views when saying most collaborations focused on training and improving referrals.
Sub-theme 1.2. Negative perspective on collaboration when treating epilepsy
The findings of this study revealed that some faith-based healers believe it is impossible to collaborate with healthcare professionals because their management is entirely different, and they don’t believe that epilepsy can be cured medically. They were also concerned considering the poor relationship they have had in the past. The findings were elaborated on the following quotes:
“Epilepsy is caused by witchcraft, so it can only be treated traditionally. Doctors can treat other medical conditions which require medical treatment. Its impossible to work with doctors”. “I can’t share my indigenous language with anyone. I fell sick when I had a calling to train in traditional healing, and it was painful. If I share my indigenous knowledge with doctors, they will use it to manufacture their medical treatment” (Male, 54 years old).
“Honestly, I don’t ever wish to work with doctors. There is a lot of information that they do not have regarding the management of epilepsy. I think they should work as a medical team and not get involved in the kind of management we provide”. Lack of resources also came up as a category of barrier to collaboration” (Female, 35 years old).
There was mutual distrust and skepticism among the two groups.
Theme 2. Strategies to enhance implementation of collaboration / Тема 2. Стратегии по улучшению реализации сотрудничества
The findings of this study indicated that traditional healers have their own desired strategies on how collaboration between traditional healers and health professionals can be done. Traditional healers believe that there should be mutual respect for collaboration to work. If the patient has epilepsy due to spiritual root cause, then the treatment will be spiritual; if the causes are medical, then the treatment will be medical. Traditional healers suggested that patients should consult them first then they will refer to the health facility if it is necessary and would expect medical practitioners to refer them back.
Sub-theme 2.1: Mutual referral system
Participants explained that they always referred patients to the hospital for appropriate management as they acknowledged that medical treatment can be effective. The following quotes elaborate on the findings:
“PLWE should consult us first; then we will diagnose and treat the disease if it requires spiritual treatment, then we will refer the patients to the hospital for further management. The doctors should also refer the clients if they cannot treat the disease medically” (Male, 55 years old).
“It is possible to work with health professionals. I can refer the patients to the hospital if the causes are not spiritual, but the doctors must also refer some patients to me so that they receive adequate treatment for spiritual epilepsy” (Male, 60 years old).
However, the preferred referral system was mainly one-sided, with traditional healers referring patients to medical practitioners and not the other way around.
Sub-theme 2.2. Creation of opportunities for consultation rooms accessibility within the health facility
Traditional healers believed that they should have accessibility within the health facility through their consultation rooms to work with the health professionals efficiently. Furthermore, they indicated that they want to be allocated to work in Out Patient Department to assist the health professionals in sorting the patients according to the required treatment. The findings were supported by the following quotes:
“The government should give us a chance to work with doctors at the hospital to assist them in diagnosing and identifying the patient who require traditional healing. The government doesn’t recognise us at all” (Female, 36 years old).
“I would work with medical doctors on condition that they acknowledge that we both have the necessary knowledge and skills to manage epilepsy so they should respect my calling and my ancestors as well”. (Male, 60 years old).
“Traditional healers must have their hospital consultation rooms so that the PLWE can access their preferred treatment method without any struggle” (Female, 57 years old).
For collaboration to work, there is a need to recognise mutual respect and commitment from the government to provide the necessary support and financial resources.
DISCUSSION / ОБСУЖДЕНИЕ
Findings show that traditional healers were not aware of any formal collaboration. The majority of traditional healers were willing to collaborate with healthcare professionals, which would highly improve the management of epilepsy as well as the quality of life of people living with epilepsy. Collaboration should be a two-way process, and not only traditional practitioners refer but the medical practitioners are not referring the clients. There is a need for mutual respect for collaboration to work.
Based on the findings, it can be assumed that the management of epilepsy can be improved through collaboration, as traditional healers were willing to enhance their capacity and make referrals to health facilities. It is believed that most PLWE will have access to early diagnosis and appropriate treatment, improving the quality of life as they will be treated holistically.
These findings were supported by L. Deuchar et al. [6] who indicates that in Kenya, most practitioners (including traditional healers, faith healers and health professionals) were willing to collaborate and acknowledged the benefits of collaboration. Furthermore, a study in South Africa found that traditional healers and biomedical practitioners felt that collaboration could provide more culturally appropriate treatment for PLWE [6]. In addition, WHO [2] revealed that traditional healers could also offer a more culturally acceptable, less stigmatised and more varied treatment approach consistent with PLWE’S beliefs about the causes of epilepsy. Hence, collaboration with health professionals would be quite beneficial as traditional healers are considered the primary care providers by most of PLWE. Traditional healers in Congo were willing to collaborate with trained health professionals to manage epilepsy. Given the strong influence of traditional healers and the persistence of epilepsy-related stigma, such collaboration should be considered [14].
The mutual respect and understanding of collaboration provide a good ground for the initiation and implementation. Traditional healers and health professionals can freely share ideas on how the collaboration can be successful in helping improve the quality of life for PLWE. Therefore the, collaboration requires all stakeholders to have good interpersonal relations characterized by mutual respect and an ongoing flow of knowledge and insights. In contrast, few traditional healers in this study were unwilling to collaborate with health professionals due to their beliefs regarding the causes and management of epilepsy. They believe that epilepsy is a spiritual disease, therefore the management should also be spiritual and that health professionals cannot manage or treat epilepsy.
According to this study's findings, most traditional healers acknowledge that collaboration can greatly reduce the epilepsy treatment gap and improve the quality of life of PLWE. Interestingly, they have great ideas on how the collaboration can be initiated and implemented, showing a positive attitude. Similarly, E. Krah [5] also found that traditional healers preferred a more integrated system, suggesting that access to rooms in health facilities would facilitate collaboration. WHO [15] calls for better integrating traditional medicine into national primary care systems. Traditional healers interpreted this as having consultation rooms within the health care facilities.
Furthermore, they explained that it would be best for them to be allocated in the outpatient department so that they can sort the patients according to the kind of treatment required by specific PLWE (triage). This means that the traditional healers advocate for the government to permit them to have their consultation rooms built within the hospital facilities where they can diagnose and treat PLWE. The consultation rooms are to be designed according to the required cultural standards. However according to the Traditional Health Practitioners Act 22 of 2007 [16], no mention of consulting rooms at health facilities. According to the Act, traditional healers' practice must be regulated to ensure patients’ safety.
B. Green and E. Colucci [17] also found that some traditional healers would like training to understand how health professionals diagnose and treat epilepsy. Furthermore, study participants expressed that healers should be educated and be able to identify the symptoms of mental illness, including epilepsy and to distinguish what they could treat and when to refer to Western healthcare facilitie. Traditional healers expressed interest in training to improve their patient management skills, indicating that they would be “willing to attend workshops organised by the government [17].
In addition, M.J. Keikelame and L. Swartz [18] corroborated that traditional healers supported collaboration with health professionals. They also emphasised that the approach must have official agreements regarding protecting intellectual property, accountability and respect of their indigenous knowledge. Collaboration can be initiated through a mutual referral system, dialogue, training, and respect [18].
The mutual agreement can be developed by policymakers who will then liaise with other relevant stakeholders to ensure that the agreement can accommodate both modern health systems an traditional healing systems.
Most traditional health practitioners were willing to collaborate mainly with primary health care providers through referring cases. A system of co-referral seemed preferable. To initiate the referral process, the traditional healers should be educated on the diagnosis of epilepsy so that they can refer PLWE to health professionals for appropriate management. For the approach to the effective, all stakeholders are required to have significant social interactions to promote good communication.
Based on the findings, it can be concluded that there is a need for capacity building, mutual respect, and co-referral as collaboration to manage epilepsy effectively. It was motivating to note that most traditional healers were willing to collaborate, capacitated and have valuable ideas on making it successful. The collaboration would be highly favourable to PLWE because it will minimise the confusion regarding the treatment choice and promote early diagnosis and treatment, improving the quality of life.
Acknowledgements / Благодарности
Researchers would like to acknowledge the traditional healers from rural villages of Mpumalanga and Limpopo provinces for participating in the study, The GladAfricas Foundation Trust and The Council for Scientific and Industrial Research (CSIR) for funding the study. The village chiefs for providing permission to access the villages.
CONCLUSION / ЗАКЛЮЧЕНИЕ
Although few traditional healers were not willing to collaborate. Most traditional healers were eager to collaborate with health professionals and acknowledged the collaboration's significance. They cited a mutual referral system, training, dialogue, and respect. Therefore, collaboration between health professionals and traditional services could allow for the transfer of skills and knowledge hence improving the management of epilepsy.
There is a need to develop guidelines that will enhance the implementation of collaboration by enhancing mutual respect, mutual referral system, dialogue, and training. Training could assist with understanding how epileptic drugs work to maintain adherence. Nevertheless, there is limited literature regarding negative perspectives on epilepsy management collaboration.
1. Nemathaga M. Cultural congruent interventions for epilepsy in the selected rural communities of Limpopo and Mpumalanga Provinces (2022).
References
1. Boumediene F., Chhour C., Chivorakoun P., et al. Community-based management of epilepsy in Southeast Asia: Two intervention strategies in Lao PDR and Cambodia. Lancet Reg Health West Pac. 2020; 4: 100042. https://doi.org/10.1016/j.lanwpc.2020.100042.
2. World Health Organization. Epilepsy. 9 February 2023. Available at: https://www.who.int/news-room/fact-sheets/detail/epilepsy (accessed 05.06.2023).
3. Das G., Biswas S., Dubey S., et al. Perception about etiology of epilepsy and help-seeking behavior in patients with epilepsy. Int J Epilepsy. 2021; 7 (1): 22–8. https://doi.org/10.1055/s-0041-1731933.
4. Kwedi Nolna S., Ntonè R., Fouda Mbarga N., et al. Integration of traditional healers in human African trypanosomiasis case finding in central Africa: a quasi-experimental study. Trop Med Infect Dis. 2020; 5 (4): 172. https://doi.org/10.3390/tropicalmed5040172.
5. Krah E., de Kruijf J., Ragno L. Integrating traditional healers into the health care system: challenges and opportunities in rural northern Ghana. J Community Health. 2018; 43 (1): 157–63. https://doi.org/10.1007/s10900-017-0398-4.
6. Solera-Deuchar L., Mussa M.I., Ali S.A., et al. Establishing views of traditional healers and biomedical practitioners on collaboration in mental health care in Zanzibar: a qualitative pilot study. Int J Ment Health Syst. 2020; 14: 1. https://doi.org/10.1186/s13033-020-0336-1.
7. Jama N.A., Nyembezi A., Lehmann U. Evidence of past and current collaborations between traditional health practitioners and biomedical health practitioners: a scoping review protocol. BMJ Open. 2021; 11 (1): e043454. https://doi.org/10.1136/bmjopen-2020-043452.
8. Kokota D., Stewart R.C., Abbo C., Bandawe C. Views and experiences of traditional and Western medicine practitioners on potential collaboration in the care of people living with mental illness in Malawi. Malawi Med J. 2022; 34 (4): 231–8. https://doi.org/10.4314/mmj.v34i4.2.
9. De Vos A., Strydom H., Fouche C., Delport C. Research at Grass Roots: for the social sciences and human service professions. Book review. Unisa Psychologia. 2015; 29 (1): 154–8.
10. Gray J.R., Grove S.K., Sutherland S. Burns and Grove’s The practice of nursing research: appraisal synthesis and generation of evidence. 8th ed. Philadelphia: S.W Saunders; 2016: 736 pp.
11. Polit D.F., Beck C.T. Nursing research: generating and assessing evidence for nursing practice. 10th ed. Philadelphia: Wolters Kluwer Health; 2017: 784 pp.
12. Brink H. Fundamentals of research methodology for health care professionals. 3rd ed. Cape Town: Juta; 2016.
13. Creswell J.W., Creswell J.D. Research design: qualitative, quantitative, and mixed methods approaches. 5th ed. SAGE publications; 2018: 304 pp.
14. Dusabimana A., Mandro M.N., Siewe Fodjo J.N., et al. Community perceptions and attitudes regarding epilepsy and disease cost after implementation of a community-based epilepsy treatment program in onchocerciasis-endemic communities in the Democratic Republic of Congo. Epilepsy Behav. 2021; 116: 107773. https://doi.org/10.1016/j.yebeh.2021.107773.
15. World Health Organization. WHO traditional medicine strategy: 2014-2023. Available at: https://www.who.int/publications/i/item/9789241506096 (accessed 05.06.2023).
16. South African Government. Traditional Health Practitioners Act 22 of 2007. Available at: https://www.gov.za/documents/traditional-healthpractitioners-act (accessed 05.06.2023).
17. Green B., Colucci E. Traditional healers’ and biomedical practitioners’ perceptions of collaborative mental healthcare in lowand middleincome countries: a systematic review. Transcult Psychiatry. 2020; 57 (1): 94–107. https://doi.org/10.1177/1363461519894396.
18. Keikelame M.J., Swartz L. ‘A thing full of stories’: traditional healers’ explanations of epilepsy and perspectives on collaboration with biomedical health care in Cape Town. Transcult Psychiatry. 2015; 52 (5): 659–80. https://doi.org/10.1177/1363461515571626.
About the Authors
M. NemathagaSouth Africa
Muofheni Nemathaga – PhD Candidate, Department of Advanced Nursing Science, Faculty of Health Sciences
University Rd, Thohoyandou 0950
M. S. Maputle
South Africa
Maria Sonto Maputle – Professor, Department of Advanced Nursing Science, Faculty of Health Sciences
University Rd, Thohoyandou 0950
L. Makhado
South Africa
Lufuno Makhado – Professor, Department of Public Health, Faculty of Health Sciences
WoS ResearcherID: I-1586-2016; Scopus Author ID: 56224434100.
University Rd, Thohoyandou 0950
N. S. Mashau
South Africa
Ntsieni Stella Mashau – Associate Professor, Department of Public Health, Faculty of Health Sciences
University Rd, Thohoyandou 0950
Review
For citations:
Nemathaga M., Maputle M.S., Makhado L., Mashau N.S. Views of traditional healers on collaboration with health professionals when managing epilepsy in rural areas of Limpopo and Mpumalanga Provinces (South Africa). Epilepsy and paroxysmal conditions. 2023;15(3):222–231. https://doi.org/10.17749/2077-8333/epi.par.con.2023.165
JATS XML

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.










































