Scroll to:
Migraine manifestations due to correction of secondary hyperhomocysteinaemia
https://doi.org/10.17749/2077-8333/epi.par.con.2025.217
Abstract
Migraine is one of the most common causes of headache with the prevalence reaching 21% and 6% in females and males, respectively, thereby attracting a great attention in investigating underlying migraine pathogenesis. The current article presents a clinical case of alleviated migraine manifestations in female patient with verified hyperhomocysteinaemia occurred due to severe folic acid deficiency. The additional specific characteristic of this case is associated to asymmetry of venous sinuses, revealed by contrast-free magnetic resonance angiography that accounts for cerebral venous dyscirculation. Hyperhomocysteinaemia is one of the factors of endothelial dysfunction, which impact in different diseases, including cerebrovascular, is being discussed. The data have been collected evidencing about a more frequent incidence of this disorder among patients with migraine than in healthy volunteers. Because hyperhomocysteinaemia may be decreased by medical therapy, it’s detection and correction potentially may alleviate migraine manifestations. This hypothesis require to be further investigated.
For citations:
Bedenko A.S. Migraine manifestations due to correction of secondary hyperhomocysteinaemia. Epilepsy and paroxysmal conditions. 2025;17(1):54-58. https://doi.org/10.17749/2077-8333/epi.par.con.2025.217
INTRODUCTION / ВВЕДЕНИЕ
Migraine is a common cause of headache, its prevalence reaches 21% and 6% in women men, respectively, more frequently occurs only tension headache in primary causes of cephalgia [1]. Currently, a periodically occurring neurogenic aseptic inflammation of the small vessel wall in the dura mater has been generally accepted as a migraine pathophysiological concept [1][2].
A special place in the study of migraine pathogenesis is held by search for biomolecules associated with developing headaches in migraine and its other manifestations. Sometimes, as in the case of the calcitonin gene-related peptide (CGRP), the identification of such biologically active substance leads to a fundamentally new therapeutic strategy [2], but more often an increase in level of certain biomolecules results in no crucial change in therapeutic approaches. Thus, some studies have demonstrated that during a migraine attack the level of cytokines, pentraxin-3 and metalloproteinase-9 [3] becomes elevated thereby clearly confirming the concept of neurogenic aseptic inflammation, but can hardly lead to dramatically new therapeutic approaches.
In this regard, scientific interest has been primarily focused on investigating metabolic aberrations in migraine, which detection and correction may be applied in wide clinical practice and, accordingly, successfully implemented in the medical care protocols for migrainious patients. Potentially, homocysteine (a sulfur-containing amino acid, a methionine metabolite) may be a candidate metabolite. It is known that homocysteine is one of the factors of endothelial dysfunction, as well as atherogenesis [4] that was reported to increase in cerebrovascular diseases and some brain autoimmune disorders (multiple sclerosis) [5][6].
The article presents a patient case of improved migraine course upon correction of newly diagnosed hyperhomocysteinemia.
CASE REPORT / КЛИНИЧЕСКИЙ СЛУЧАЙ
Patient P., born in 1987, applied to a neurologist in out-patient center with complaints of bilateral headaches (7–8 points by visual analogue scale (VAS)) that may be accompanied by nausea, dizziness (without any sense of rotation) at the peak of pain attack, and intermittent tinnitus. Vomiting, photo-, and phonophobia were not observed.
Anamnesis / Medical history
Patient P. suffers from cephalgic syndrome many years. The worsening was noticed every 3–4 weeks: headaches became quotidian, bilateral, most severe in mornings, accompanied by nausea, and increased with physical exertion. The severity of the pain syndrome varied from 5 to 8 points by VAS. Previously, estrogen-containing therapy was noted to exacerbate cephalgic syndrome. At the time of apply to the doctor, the patient took daily the standard combination of painkillers (acetylsalicylic acid + paracetamol + caffeine). Anamnesis of life reports that endometrioid cyst was removed in 2014.
Neurological status / Неврологический статус
At the time of examination, no general cerebral, focal or meningeal symptoms were observed.
Preliminary diagnosis / Предварительный диагноз
Taking into account the clinical and anamnestic data, the preliminary diagnosis was formulated as: "Cephalgic syndrome of complicated origin (cerebral venous dysgemia + tension headache). Differential diagnosis with transformed migraine."
The patient was recommended additional examination to exclude or verify secondary cephalgias.
Instrumental examinations / Инструментальные исследования
According to brain magnetic resonance imaging (MRI) and magnetic resonance venography (1.5 T with contrast enhancement), no pathological foci were found. Asymmetry of the transverse and sigmoid sinuses without signs of thrombosis was revealed (Fig. 1).
According to the results of brachiocephalic artery ultrasound examination and transcranial Doppler sonography, no ultrasound signs of vascular pathology in the Willis circle were revealed at the time of the study. Indices, characterizing peripheral vascular resistance, were within normal range. The non-linear pattern of the vertebral arteries between the transverse processes of the cervical vertebrae is obviously due to general spine degenerative disease.
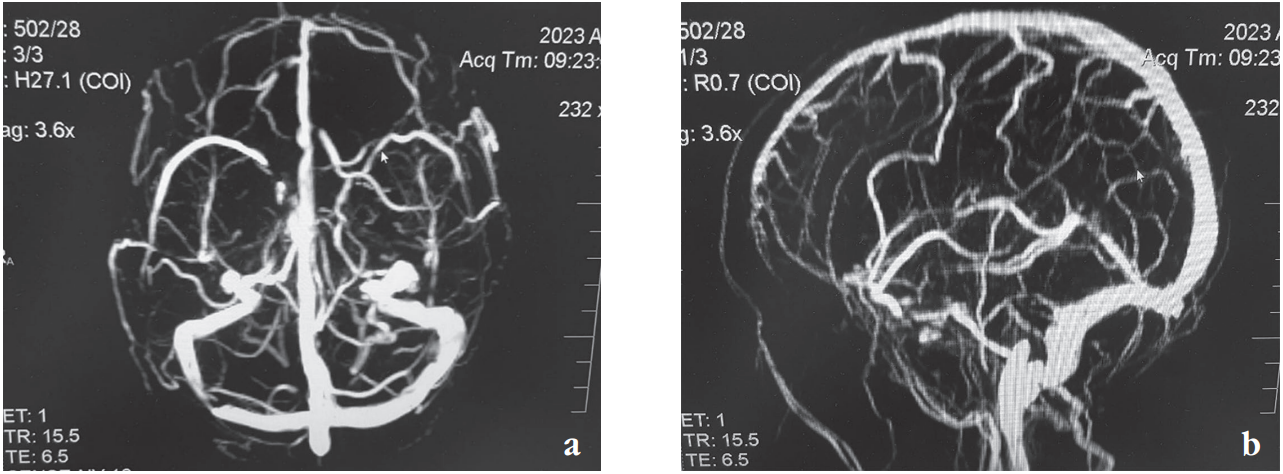
Figure 1. Magnetic resonance venography of intracranial sinuses: а – axial plane; b – sagittal plane
Рисунок 1. Магнитно-резонансная венография внутричерепных синусов: а – аксиальная проекция; b – сагиттальная проекция
Laboratory tests / Лабораторные исследования
No pathological changes were found in clinical blood test. The general coagulation factor levels were unaltered. A blood serum homocysteine test revealed hyperhomocysteinaemia (25.35 μmol/l). The patient was referred to a hematologist, who advised additional laboratory tests.
No alteration in general coagulogram were identified: D-dimer 110.41 ng/ml; fibrinogen 2.91 g/l; prothrombin time 11.4 sec; international normalized ratio 1.05; activated partial thromboplastin time 23.1; thrombin time 13.6 sec; antithrombin III 105%; lupus anticoagulant 0.73 c.u.; protein C 76% and protein S 84.5% (within normal range). A profound folic acid deficiency was detected – 2 ng/ml (vitamin B12 – 311 pg/ml, which corresponds to normal range).
Patient K. was examined for antiphospholipid syndrome: total antibodies to cardiolipin – 6.3 U/ml, antibodies to beta-2-glycoprotein I – 12.33 U/ml, which also corresponds to normal range.
The study of some genetic factors was also performed to identify defects in folate cycle enzyme: no mutations in the MTR, MTRR, MTHFR genes were found suggesting secondary cause of hyperhomocysteinaemia.
The patient was consulted by a gastroenterologist, and a diagnosis of atrophic gastritis was established.
Therapy / Терапия
Zolmitriptan orally at a dosage of 2.5 mg was prescribed as a measure for relieving headache. During dynamic observation, a positive triptans-related effect on headache was noted. Also, in connection with the developing abusus, therapy was carried out with intravenously administered dexamethasone dissolved in Ringer's solution according to the scheme: Day 1 – 8 mg, Day 2 – 4 mg, Day 3 – 4 mg.
After this, due to decline in homocysteine level the therapy was prescribed (angiovit, 2 tablets twice a day for 1 month), as well as a drug containing diosmin and hesperidin with positive effect on venous wall condition. While taking this drug, the frequency of headaches decreased from everyday pain to 10–15 days per month. A control examination revealed lowered homocysteine level down to 7.29 μmol/l, which corresponds to normal range.
Final diagnosis / Окончательный диагноз
Based on complaints, anamnestic and clinical data, laboratory and instrumental examinations, the final diagnosis was formulated as follows: predominant diagnosis: “Migraine without aura with daily attacks, decompensation”.
Secondary diagnosis: “Cerebral venous dysgemia, intracranial sinus asymmetry. Secondary hyperhomocysteinemia (folic acid deficiency)”.
In order to reduce the frequency of headache attacks, the patient was prescribed prophylactic therapy with venlafaxine for six months. Subsequently, the patient did not apply for medical attention; an active telephone survey a year after the initial visit revealed about personal therapy cessation 4 months later due to the onset of stable remission. Repeated monitoring of folic acid and homocysteine levels was not performed.
DISCUSSION / ОБСУЖДЕНИЕ
The patient was diagnosed with migraine according to the international migraine criteria [7]:
a) at least 5 attacks fulfilling criteria b–d;
b) headache attacks lasting 4–72 hours (when untreated or unsuccessfully treated);
c) headache has at least two of the following four characteristics: unilateral localization, pulsating character, moderate or severe pain intensity, aggravation by or causing avoidance of routine physical activity (e.g., walking or climbing stairs);
d) during headache at least one of the following: nausea and/or vomiting; photophobia and phonophobia;
e) not better accounted for by another Classification of Headache Disorders, 3rdrevision diagnosis.
The features of the presented clinical case are an increased homocysteine level, as well as structural changes in the intracranial sinuses, contributing to developing cerebral venous dyscirculation.
Endothelial dysfunction is the general pathophysiological mechanism in multiple diseases. The data on higher probability of developing cardiovascular diseases in patients with migraine (especially migraine with aura) most likely due to endothelial dysfunction are recognized. This hypothesis is confirmed by the results from several studies: a higher level of endothelin-1 in patients with migraine, increased platelet activating factor and von Willebrand factor levels during migraine attack [1][3].
Homocysteine is one of the well-studied factors resulting in endothelial dysfunction. However, presuming homocysteine level increase in migraine is contradictory. Some studies revealed higher cerebrospinal fluid homocysteine level in migraine compared to control group [8], whereas others found increased blood plasma homocysteine levels in patients with migraine with aura compared to control group [3][9]. On the other hand, no significant relationship between migraine and hyperhomocysteinemia was reported [3]. Meanwhile, while highlighting results of meta-analyses as more reliable source, it is worth mentioning the meta-analysis published in 2020 by the American Headache Society showing a positive relationship between hyperhomocysteinemia and migraine [10]. It is noteworthy that it also presents the data from several independent studies demonstrating that plasma folate levels are lower in migraine patients compared to healthy volunteers.
Hyperhomocysteinemia can be either secondary (due to folic acid or vitamins B12, B6 deficiency) or primary, genetically determined. Several genes (mainly in the folate cycle) have been identified, mutations in which result in developing hyperhomocysteinemia. In patient P. presented here, hyperhomocysteinemia turned out to be secondary, caused by folate deficiency. Meanwhile, it should be noted that hereditary hyperhomocysteinemia often occurs as a result of a mutation in the methylenetetrahydrofolate reductase (MTHFR) gene. According to some studies, the frequency of such a mutation among migraine-suffering children reaches 53.3% [11]. Several independent studies have demonstrated that migraine patients were more likely to be homozygous for the MTHFR C677T allele (point missense mutation) compared to general population [3]. Finally, Z.G. Tadtaeva et al. (2021) concluded that mutations in several folate cycle genes (MTHFD1, MTHFR, MTRR, MTR) can be considered as migraine-associated markers [11].
CONCLUSION / ЗАКЛЮЧЕНИЕ
Endothelial dysfunction is one of the general pathophysiological mechanisms in various nosologies, and an increase in homocysteine level is one of the grounds in the formation of this condition. There have been accumulated the data indicating a more frequent occurrence of hyperhomocysteinemia in patients with migraine than in general population. Unlike many other factors underlying endothelial dysfunction, hyperhomocysteinemia responds well to correction with vitamin B therapy. In the presented case report, an improvement in migraine course (a return to migraine attacks instead of chronic one) was noted upon hyperhomocysteinemia correction. Therefore, it allows to suggest that detection and correction of such disorders in patients with migraine can lead to improved course of the disease, but further larger scale studies are required.
References
1. Tabeeva G.R. Migraine-associated cerebrovascular disorders. Meditsinskiy sovet / Medical Council. 2017; 10: 32–5 (in Russ.). https://doi.org/10.21518/2079-701X-2017-10-32-35.
2. Azimova Yu.E., Amelin A.V., Alferova V.V., et al. Clinical guidelines “Migraine”. S.S. Korsakov Journal of Neurology and Psychiatry. 2022; 122 (1-3): 4–36 (in Russ.). https://doi.org/10.17116/jnevro20221220134.
3. Demartini C., Francavilla M., Zanaboni A.M., et al. Biomarkers of migraine: an integrated evaluation of preclinical and clinical findings. Int J Mol Sci. 2023; 24 (6): 5334. https://doi.org/10.3390/ijms24065334.
4. Efimov V.S., Ozolinya L.A., Kazhesheva A.Z., Makarov O.V. Hyperhomocysteinemia in clinical practice. Мoscow: GEOTAR-Media; 2013: 79 pp. (in Russ.).
5. Cordaro M., Siracusa R., Fusco R., et al. Involvements of hyperhomocysteinemia in neurological disorders. Metabolites. 2021; 11 (1): 37. https://doi.org/10.3390/metabo11010037.
6. Dubchenco E.A., Ivanov A.V., Boyko A.N., et al. Hyperhomocysteinemia and endothelial dysfunction in patients with cerebral vascular and autoimmune diseases. S.S. Korsakov Journal of Neurology and Psychiatry. 2019; 119 (11): 133–8 (in Russ.). https://doi.org/10.17116/jnevro2019119111133.
7. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018; 38 (1): 1-211. https://doi.org/10.1177/0333102417738202.
8. Isobe C., Terayama Y. A remarkable increase in total homocysteine concentrations in the CSF of migraine patients with aura. Headache. 2010; 50 (10): 1561–9. https://doi.org/10.1111/j.1526-4610.2010.01713.x.
9. Moschiano F., D’Amico D., Usai S., et al. Homocysteine plasma levels in patients with migraine with aura. Neurol Sci. 2008; 29 (Suppl. 1): S173–5. https://doi.org/10.1007/s10072-008-0917-2.
10. Liampas I., Siokas V., Mentis A.A., et al. Serum homocysteine, pyridoxine, folate, and vitamin B12 levels in migraine: systematic review and meta-analysis. Headache. 2020; 60 (8): 1508–34. https://doi.org/10.1111/head.13892.
11. Tadtaeva Z.G., Yakovleva E.E., Amelin A.V. Polymorphism of methylenetetrahydrofolate reductase (MTHFR) folate metabolism gene and hyperhomocysteinemia in migraine. Patologicheskaya fiziologiya i eksperimental’naya terapiya / Pathological Physiology and Experimental Therapy. 2021; 65 (4): 109–15 (in Russ.). https://doi.org/10.25557/0031-2991.2021.04.109-115.
About the Author
A. S. BedenkoRussian Federation
Anna S. Bedenko, PhD
Scopus Author ID: 57220812877
16 Krasnaya Presnya Str., Moscow 123242
Review
For citations:
Bedenko A.S. Migraine manifestations due to correction of secondary hyperhomocysteinaemia. Epilepsy and paroxysmal conditions. 2025;17(1):54-58. https://doi.org/10.17749/2077-8333/epi.par.con.2025.217

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.











































