Scroll to:
Terminology of medicines used to control seizure disorders: 2024 ILAE Recommendations and profile of real-world term use
https://doi.org/10.17749/2077-8333/epi.par.con.2024.209
Abstract
Background. The International League Against Epilepsy (ILAE) has provided recommendations on the terminology of medicines for control of seizure disorders, which should be adapted into different languages.
Objective: to evaluate the usage profile of terms describing the effects of medicines used in patients with epilepsy.
Material and methods. The search query analysis systems Google Trends and Yandex Wordstat as well as PubMed/MEDLINE, Google Scholar and eLibrary databases were used to evaluate the general public and professional usage profile, respectively.
The following terms in Russian and English were studied: “antiepileptic”, “antiepileptic drug”, “antiseizure”, “antiseizure drug”. In order to ascertain a prevailing opinion within professional and patient communities, a questionnaire survey was conducted on the public online resources of the non-profit partnership “The Association of Epileptologists and Patients” carried out via the cloud-based cross-platform social media as well as instant messaging service Telegram and the social media platform VK.
Results. In the English-speaking internet segment, the term “antiepileptic” is used more than 5 times frequently than “antiseizure” by the general public. Conversely, in the Russian-language segment, the term “antiseizure” is almost 2.5 times more common. The term “antiepileptic” is more prevalent in scientific community in both segments. This finding aligns with the profile of terminology usage observed among epileptologists and epilepsy patients. The questionnaire survey results revealed that 56.42% of 179 respondents were in favor of the terms “antiepileptic drug”, “AED” and “antiepileptic therapy”, whereas as few as 17.32% of those endorsed the ILAE-proposed terminology.
Conclusion. In light of the established practice of terminology use in both professional scientific community and among practicing epileptologists and epileptic patients, as well as the differences in the semantics of English- and Russian-language terms and the identified lack of precision in the ILAE definition of epilepsy, it can be concluded that for the Russian-speaking population, the terms “antiepileptic drug”, “AED” are more preferable rather than the terms “antiseizure medication”, “ASM”. Additionally, it is preferable to use the terms “convulsive ictus” and “epileptic ictus” due to negative connotation with term “seizure” in Russian. The terms “antiseizure” and “antiepileptic” should not be regarded as mutually exclusive in the context of treatment that has a direct impact on epilepsy course. Finally, it is necessary to further refine epilepsy definition and classification.
Keywords
For citations:
Blinov D.V., Petrukhin A.S., Voronkova K.V., Akarachkova E.S., Kotova O.V., Mnatsakanyan A.N., Kurchatkina G.P. Terminology of medicines used to control seizure disorders: 2024 ILAE Recommendations and profile of real-world term use. Epilepsy and paroxysmal conditions. 2024;16(3):176–191. https://doi.org/10.17749/2077-8333/epi.par.con.2024.209
INTRODUCTION / ВВЕДЕНИЕ
Terminology related to drugs used in the treatment for patients with epilepsy is a subject of debate in the medical community. The terms “antiepileptic”, “antiepileptic drug” (AED), “antiseizure”, “antiseizure drug” (ASD), as well as “anticonvulsant”, “anticonvulsant therapy”, “anticonvulsant drug”, are used in the Russian language. In English, the terms “antiepileptic drug” (AED) and “antiseizure drug”, “antiseizure medicines” (ASM), “anticonvulsant” are used respectively. Although these terms are often considered interchangeable both in English and in Russian, there is a difference in their semantic meaning.
The proponents of the term “antiepileptic” claim that it covers a wider range of therapeutic effects beyond the exclusive control of seizures. These drugs not only suppress seizures, but also have a modulating effect, contributing to the relief of concomitant symptoms, including cognitive impairment, mood disorders and neuropathic pain, thus improving the overall quality of life (QoL). The experts supporting the term “antiseizure” argue their preferences by specificity of the core pharmacological action of these drugs: suppression of seizures.
In January 2024, the International League Against Epilepsy (ILAE) released a document outlining their position on the issue [1].
2024 ILAE recommendations / Рекомендации МПЭЛ 2024
The ILAE position was formed under the auspices of the Nomenclature Task Force with the representation from all ILAE regions, the International Bureau for Epilepsy (IBE) and from the experts with both clinical and basic scientific research experience. As in previous ILAE documents preparation, a modified Delphi process was applied [2–7].
The accepted statements with the assigned score served as the basis for the draft of the initial version of the consensus document, which was then submitted to the Executive Committee of the ILAE. After review by the Executive Committee, the document was submitted to the journal Epilepsia for peer review and simultaneously placed on the ILAE website1 for public review. The ILAE position was finalized after taking all comments of the reviewers of the journal and the visitors to the official website into account.
The following are the recommendations of the ILAE [1].
Recommendation 1. “Antiseizure” as preferred term for medications having a symptomatic effect
There was consensus within the Task Force that most medications currently used to treat epilepsy exert their effects by suppressing symptoms (seizures). In fact, these medications have been approved by regulatory authorities based solely on the evidence of a symptomatic effect on seizure activity. Therefore, the term “antiseizure” is the most appropriate term to describe these medications. The Task Force considered that the term “antiseizure” is sufficiently explanatory in the English language, and that including the term “epileptic” when describing the effect of these medications is redundant in this language.
Recommendation 2. “Seizure” versus “epileptic seizure”
Although the term “seizure” in the English language is used predominantly in the context of epileptic seizures, the same term has been applied also to indicate psychogenic non-epileptic seizures (PNES), currently renamed functional/dissociative seizures (FDS) [8–11].
PNES/FDS are paroxysmal events that might be mistaken for epileptic seizures. However, their underlying neurobiology differs from that of epileptic seizures and is likely to reflect a complex episodic brain network dysfunction not involving epileptic activity [12]. Although initially, the Nomenclature Task Force proposed that the term “seizure” should be reserved preferably to indicate epileptic seizures, feedback from public comments showed that no consensus could be reached on this proposition. Consequently, following further consultation within the ILAE membership, including the ILAE Task Force on FDS, it was agreed that the term “seizure” can also be applied to non-epileptic events. When the term “seizure” describes PNES/FDS, the context must clearly distinguish these events from epileptic seizures to reduce the risk of confusion.
ASMs act to suppress epileptic seizures by modulating neuronal excitability through their actions on receptors, ion channels, and other molecules. These actions link them to the neurobiology of epileptic seizures as manifestations of abnormal excessive or synchronous neuronal activity in the brain [13]. When applied to these medications, “antiseizure” refers to epileptic seizures. Because of their complex pharmacology, some ASMs can also be effective in other indications, such as neuropathic pain, psychiatric disorders, and migraine.
A diagnosis of PNES/FDS does not warrant the use of ASMs unless epileptic seizures co-exist. Well-established treatments for PNES/FDS consist of a well-structured explanation of the diagnosis, psychoeducation, psychological therapies, and, sometimes, antidepressants or other psychoactive drugs (including certain ASMs) that target mood or anxiety disorders [10, 14].
Recommendation 3. “Medication” versus “medicine” or “drug”
The Task Force also discussed alternatives to the term “medication”.
“Medication” in the English language refers only to therapeutic products, whereas “medicine” is used to indicate both the science of treating symptoms/diseases as well as the products used to treat these conditions. This may justify a preference for the term “antiseizure medication” (ASM), although both “medication” and “medicine” can be used interchangeably in this context.
On the other hand, the term “antiseizure drug” (ASD) is not recommended because the acronym “ASD” is widely established to indicate autism spectrum disorder and is also used in cardiology as acronym for atrial septal defect.
Recommendation 4. When should the term “antiepileptic” be used?
Use of the term “antiepileptic” is not recommended when describing medications that have a purely symptomatic effect. The Task Force acknowledged that a medication that alters the symptom of seizure, by providing seizure control (including suppression of epileptic electroencephalography (EEG) discharges), can have an indirect favorable impact on other outcomes such as cognitive development and, possibly, susceptibility to further seizures. Any such favorable effect on the underlying disease, however, could be solely a consequence of symptom suppression. In fact, using the term “antiepileptic” in this setting may mislead people with epilepsy, their caregivers, the lay public, and health care professionals into believing that these medications treat more than just the symptoms of the disease and that the disappearance of the symptoms could necessarily signal disappearance of the underlying disease.
The Task Force initially suggested that the term “antiepileptic” be reserved for medications that have been demonstrated to directly affect the course of epilepsy, the likelihood of developing epilepsy, or the likelihood of developing more severe epilepsy. However, based on feedback from the public consultation, the Task Force agreed that using the label “antiepileptic” is undesirable because of stigma-related implications and the possibility that it could be misinterpreted as meaning “against a person with epilepsy.” This term could also create confusion with earlier literature where the term “antiepileptic” was applied to medications having a symptomatic effect on seizures.
Applying the term “antiseizure” to treatments that have symptomatic effects does not exclude that the same treatments may have, in addition, direct actions on the underlying epilepsy, epileptogenic processes, or co-morbidities. For example, a medication could have antiseizure effects and have an independent effect on epileptogenesis. Therefore, “antiseizure” and “antiepileptic” (or whatever term is chosen to indicate treatments with direct effects on the course of the disease) should not be regarded as being mutually exclusive. The provision of recommendations on the terminology to be used for treatments that are not purely symptomatic is beyond the purpose of the paper [1].
Recommendation 5. Application to non-pharmacological treatments
In addition, appropriate terminology should be used to describe not only pharmacological treatments (medications), but also the actions of other therapeutic modalities such as surgery, neurostimulation, and dietary treatments. However, providing specific recommendations on this topic is beyond the purpose of the article [1].
Recommendation 6. Language-specific issues
Although the Task Force's remit was to develop recommendations for English-language terminology, there is a need for a similar efforts to be applied to the development of correct terminology in all other languages. Accordingly, ILAE encourages the development at the regional and national level of corresponding terminology in languages other than English, considering the specific social and cultural context and the need for broad stakeholders' involvement.
Rationale for considerate adaptation to the Russian language / Обоснование необходимости осмотрительной адаптации на русский язык
In its 2024 recommendations, the ILAE proposes to replace the still widely used term “antiepileptic drug” for “antiseizure medication”, arguing this idea mainly by a more accurate description of the main mechanism of action, the symptomatic effect of the drug on seizures rather than revealing the etiological impact to epilepsy itself. The ILAE emphasizes that adaptation to other languages is to be introduced with the involvement of not only healthcare professionals, but also the patient community, since the terminology should be made straightforward to the general public.
Indeed, there are a number of differences in terminology in the Russian language. So, in English, the word “drug” implies not only “medicinal product”, but is also used to refer to narcotic drugs and related activities (e.g. “drug dealer”). Another example is the word "seizures" that can be translated in different ways, as “seizures”, “convulsions”, “convulsive seizures”. Therefore, in order to clarify recommendations on the use of the terms “antiseizure” and “antiepileptic” in Russian, it is necessary to eliminate the gap in understanding of which of them and how often they are used by the general public, as well as by certain groups in professional community involving experts researching epilepsy, practicing epileptologists and neurologists along with the epilepsy patient community.
Objective: to evaluate the application profile of the terms denoting the effect of drugs used in patients with epilepsy.
MATERIAL AND METHODS / МАТЕРИАЛ И МЕТОДЫ
Taking Recommendation 6 of the ILAE into account, it is necessary to assess how often the terms in question are used both by the general public, and in professional scientific community, namely, among practicing epileptologists and in patients with epilepsy.
Current usage practice analysis / Анализ сложившейся практики использования
To evaluate the usage profile in the broad masses of population, regardless of the degree of involvement in the context of epilepsy, the following systems of search queries analysis in search engines rated among leaders in the number of daily users involved were used: Google (USA) for the speakers of English, and Yandex (Russia) for those speaking Russian (Google Trends2 and Yandex Wordstat3, respectively). The assessment was carried out with the use of the search queries “antiepileptic”, “antiseizure”, “anticonvulsant”, in English and in Russian, respectively.
Google Trends analyzed the dynamics of query popularity – the level of interest in the topic in relation to the highest indicator in the table for a certain region and time period. We evaluated the data around the world (regions were not allocated), the last 5 years were taken as the time period (from March 1, 2019 to February 29, 2024), 100 points meant the highest level of popularity of the query, 50 points – the level of popularity of the query, half as much as in the first case, 0 points meant location with insufficient data on the request under consideration.
Yandex Wordstat estimated the number of requests, the share of all requests, while also considering the data around the world without allocating any regions; the last 5 years were taken as the time period (from February 1, 2019 to January 30, 2024).
To evaluate the application profile in professional medical environment of researchers in the field of epilepsy, an analysis of the number of published scientific primary sources with the use of these terms was carried out. Since a number of international scientometric databases (ISD) are currently unavailable for search queries from Russia, it is possible to use PubMed/MEDLINE4 (USA) and Google Scholar5 (USA) to analyze scientific literature in English and in Russian. Additionally, eLibrary6 (Russia) was used as a tool for the analysis of scientific sources in Russian.
Assessment in all ISD was performed for the entire time of data accumulation, on the primary sources of the last 5 years (2019–2024). In eLibrary, a morphological search was carried out in journal articles, books, conference materials, deposited manuscripts, data sets, dissertations, reports, patents and grants. Titles, annotations, and keywords were analyzed. In all ISD, the assessment was performed according to the requests “antiepileptic”, “antiepileptic drug”, “antiseizure”, “antiseizure drug”.
Survey in epileptologists and epilepsy patients / Опрос врачей-эпилептологов и больных эпилепсией
To assess the opinion of practicing epileptologists and in patient community, a survey on the basis of public online resources of the non-profit partnership “Association of Epileptologists and Patients”, the largest organization in the Russian Federation that unites both the professional medical community and the patients, was conducted with the focus on accumulation and dissemination of the most up-to-date information about the disease to improve the quality of life of those suffering from epilepsy.
The channel “Association of Epileptologists and Patients” in the instant messaging service Telegram7 (1213 subscribers) and the community “Association of Epileptologists and Patients” on the social media platform VK8 (848 subscribers) were employed. The questionnaires on both resources were posted on April 10, 2024. They included a summary of the context and the following choice for answers to the question “Which terminology do you personally consider more applicable?”:
– “antiseizure drug” (ASD), “antiseizure medication” (ASM), “anticonvilsants”, “antiseizure therapy”;
– “antiepileptic drug” (AED), “antiepileptic medication” (AEM), “antiepileptic therapy”;
– not differed, interchangeable terminology;
– undetermined / I want to see the results of the survey.
RESULTS / РЕЗУЛЬТАТЫ
Use of the terms by general public not immersed in the context / Использование терминологии не погруженными в контекст широкими массами населения
The results of profile evaluation of the search queries on “antiepileptic” and “antiseizure” in Google Trends are shown in Figure 1. The popularity of the search query “antiepileptic” was more than 5 times higher than “antiseizure”, remaining approximately at the same level for 5 years (fluctuation in early 2022 is associated with the changes introduced to the Google Trends data collection system). No sufficient data to calculate indicators to the queries posed in Russian was found in Google Trends.
The results of the profile evaluation for search queries “antiepileptic” and “antiseizure” in Yandex Wordstat are shown in Figure 2.
On average, over the past 5 years, the number of search queries for «антиэпилептический» (“antiepileptic”), «противоэпилептический» (“antiepileptic” also) and “antiseizure” amounted to 128, 6,257 and 15,890 per month, respectively. Since the queries «противоэпилептический» and «антиэпилептический» in Russian are varieties of the same query “antiepileptic” in English, it is possible to summarize them (a total of 6385 requests per month). Thus, the number of requests using the word “antiseizure” in the Russian-speaking Internet space is almost 2.5 times higher than the use of the word “antiepileptic”.
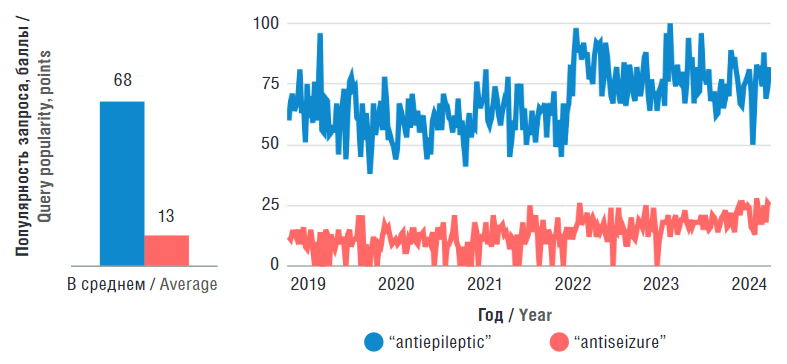
Figure 1. Evaluation results for “antiepileptic” and “antiseizure” search query profile (data source: Google Trends)
Рисунок 1. Результаты оценки профиля поисковых запросов “antiepileptic” и “antiseizure” (источник данных: Google Trends)
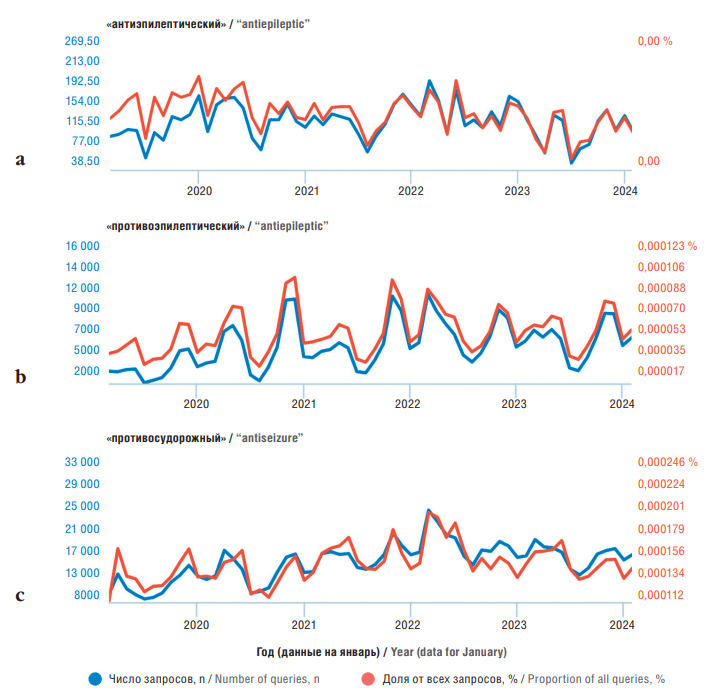
Figure 2. Dynamics for “antiepileptic” (а, b) and “antiseizure” (c) query frequency (all regions, all devices) (data source: Yandex Wordstat)
Рисунок 2. Динамика частотности запросов «антиэпилептический» (а), «противоэпилептический» (b) и «противосудорожный» (c) (все регионы, все устройства) (источник данных: Яндекс Вордстат)
Use of the terms in professional research community / Использование терминологии в профессиональном сообществе исследователей
The first work presented in PubMed/MEDLINE containing the term “antiepileptic” dates back to 1801 [15]. Since 1945, the number of publications using this term begins to number in the tens and hundreds per year, while the term “antiseizure” turned to appear in some works only since 1975 (Table 1).
Further on, the number of publications with the term “antiseizure” remains significantly less than with the term “antiepileptic". During the entire time of data accumulation in PubMed/MEDLINE, 181,753 works were identified by the search query “antiepileptic”, “antiseizure” – 5,380 works (data as of March 18, 2024). That is, the term “antiseizure” is used almost 34 times less often than “antiepileptic”. Regarding the search queries “antiepileptic drug” and “antiseizure drug” – 175496 and 3659 sources, respectively, i.e. the term "antiseizure drug" is used 48 times less frequently than “antiepileptic drug”, although recently, the disparity at evaluating “year-to-year” has been decreasing. When introducing similar queries in Russian, no correct results were obtained in PubMed/MEDLINE (Table 2).
Table 1 (beginning). Number of per-year scientific publications for “antiepileptic” or “antiseizure” search query (data source: PubMed/MEDLINE)
Таблица 1 (начало). Количество научных публикаций в год по поисковому запросу “antiepileptic” или “antiseizure” (источник данных: PubMed/MEDLINE)
Year / Год | Search query / Поисковый запрос | |||
“antiepileptic” | “antiseizure” | “antiepileptic drug” | “antiseizure drug” | |
2024 | 967 | 387 | 853 | 24 |
2023 | 4014 | 1338 | 3658 | 877 |
2022 | 4749 | 1220 | 4348 | 812 |
2021 | 4837 | 948 | 4379 | 655 |
2020 | 5064 | 519 | 4625 | 358 |
2019 | 4751 | 266 | 4338 | 181 |
2018 | 4661 | 186 | 4312 | 127 |
2017 | 4656 | 172 | 433 | 127 |
2016 | 4779 | 152 | 445 | 109 |
2015 | 4756 | 103 | 4423 | 73 |
2014 | 4884 | 77 | 4551 | 56 |
2013 | 5087 | 67 | 4768 | 51 |
2012 | 4984 | 65 | 4686 | 5 |
2011 | 4687 | 51 | 4435 | 37 |
2010 | 4486 | 52 | 4293 | 33 |
2009 | 4351 | 47 | 4161 | 35 |
2008 | 4297 | 52 | 4112 | 39 |
2007 | 4378 | 45 | 4212 | 31 |
2006 | 4088 | 40 | 396 | 31 |
2005 | 3795 | 34 | 3663 | 27 |
2004 | 3543 | 37 | 342 | 29 |
2003 | 3266 | 42 | 3174 | 28 |
2002 | 3173 | 38 | 3067 | 23 |
2001 | 3014 | 19 | 2923 | 9 |
2000 | 3148 | 25 | 3044 | 22 |
1999 | 3026 | 25 | 2937 | 14 |
1998 | 2876 | 18 | 2803 | 14 |
1997 | 2705 | 9 | 2649 | 9 |
1996 | 2743 | 14 | 2692 | 1 |
1995 | 2658 | 13 | 2623 | 1 |
1994 | 2752 | 6 | 2712 | 5 |
1993 | 2773 | 98 | 2728 | 13 |
1992 | 2754 | 14 | 2716 | 1 |
1991 | 2736 | 9 | 2709 | 8 |
1990 | 2873 | 7 | 284 | 6 |
1989 | 2761 | 7 | 2726 | 7 |
1988 | 2648 | 4 | 2629 | 3 |
Table 1 (end). Number of per-year scientific publications for “antiepileptic” or “antiseizure” search query (data source:
PubMed/MEDLINE)
Таблица 1 (окончание). Количество научных публикаций в год по поисковому запросу “antiepileptic” или “antiseizure” (источник данных: PubMed/MEDLINE)
Year / Год | Search query / Поисковый запрос | |||
“antiepileptic” | “antiseizure” | “antiepileptic drug” | “antiseizure drug” | |
1987 | 2609 | 2 | 2589 | 1 |
1986 | 2839 | 8 | 2824 | 8 |
1985 | 2755 | 3 | 2748 | 3 |
1984 | 2781 | 4 | 277 | 3 |
1983 | 2757 | 1 | 2748 | 1 |
1982 | 2444 | 3 | 2436 | 2 |
1981 | 2449 | 0 | 2447 | 1 |
1980 | 2316 | 2 | 231 | 1 |
1979 | 2342 | 1 | 2336 | 1 |
1978 | 2078 | 1 | 2076 | 2 |
1977 | 2054 | 2 | 2048 | 0 |
1976 | 202 | 1 | 2015 | 0 |
1975 | 2219 | 1 | 2217 | 0 |
1974 | 2222 | 0 | 2221 | 0 |
1973 | 2192 | 0 | 2191 | 0 |
1972 | 193 | 0 | 1928 | 0 |
1971 | 1897 | 0 | 1896 | 0 |
1970 | 1711 | 0 | 171 | 0 |
1969 | 1638 | 0 | 1635 | 0 |
1968 | 1465 | 0 | 1465 | 0 |
1967 | 1222 | 0 | 1222 | 0 |
1966 | 988 | 0 | 986 | 0 |
1965 | 961 | 0 | 961 | 0 |
1964 | 137 | 0 | 137 | 0 |
1963 | 886 | 0 | 886 | 0 |
1962 | 48 | 1 | 479 | 0 |
1961 | 369 | 0 | 369 | 0 |
1960 | 408 | 0 | 408 | 0 |
1959 | 615 | 0 | 614 | 0 |
1958 | 665 | 0 | 665 | 0 |
1957 | 589 | 0 | 589 | 0 |
1956 | 438 | 0 | 437 | 0 |
1955 | 358 | 0 | 358 | 0 |
1954 | 273 | 0 | 272 | 0 |
1953 | 26 | 0 | 259 | 0 |
1952 | 219 | 0 | 218 | 0 |
1951 | 203 | 0 | 203 | 0 |
1950 | 194 | 0 | 193 | 0 |
1949 | 157 | 0 | 156 | 0 |
1948 | 154 | 1 | 153 | 0 |
1947 | 174 | 0 | 173 | 0 |
1946 | 115 | 0 | 114 | 0 |
1945 | 26 | 0 | 26 | 0 |
1886 | 1 | 0 | 0 | 0 |
1801 | 1 | 0 | 0 | 0 |
Table 2. Number of primary sources for the search queries analyzed in international scientific databases
Таблица 2. Количество первоисточников по исследуемым поисковым запросам в международных научных базах данных
Term / Термин | PubMed/MEDLINE | Google Scholar | eLibrary | |||
All-time record / | Last 5 years / Последние 5 лет | All-time record / | Last 5 years / Последние 5 лет | All-time record / | Last 5 years / Последние 5 лет | |
«Противоэпилептический», «антиэпилептический» | – | – | ~11640 | ~3366 | 2027 | 664 |
«Противосудорожный» | –- | – | ~12500 | ~3160 | 1507 | 393 |
«Противоэпилептический препарат», «антиэпилептический препарат» | – | – | ~11690 | ~3341 | 1363 | 466 |
«Противосудорожный препарат» | – | – | ~12900 | ~3340 | 621 | 197 |
“Antiepileptic” | 181753 | 24382 | ~504000 | ~18200 | 7661 | 2388 |
“Antiseizure” | 5380 | 4678 | ~47400 | ~16900 | 924 | 719 |
“Antiepileptic drug” | 175496 | 22201 | ~422000 | ~17500 | 3572 | 1077 |
“Antiseizure drug” | 3659 | 2907 | ~38400 | ~16800 | 324 | 256 |
Only approximate data is available in Google Scholar. For the search query “antiepileptic”, this database contains approximately 504,000 results, with 18,200 over the past 5 years, for the search query “antiseizure” – 47,400 and 16,900, respectively. According to the search queries “antiepileptic drug” and “antiseizure drug” – 422,000 (of which 17,500 in the last 5 years) and 38,400 (of which 16,800 in the last 5 years) results, respectively. Thus, the term “antiseizure” is used in scientific publications posted on Google Scholar 10.6 times less often than the term “antiepileptic”, and “antiseizure drug” is 11 times less often than “antiepileptic drug". In the last 5 years, however, both terms have been used with almost the same frequency.
Google Scholar also processes search queries in Russian correctly. Within the whole period, this database has accumulated approximately 8,010 sources using the term «противоэпилептический» (translation is “antiepileptic”) and 3,630 – «антиэпилептический» (translation is “antiseizure” also), a total of 11,640, including 2,530 and 836 over the past 5 years (a total of 3,366), respectively. Use of the term “antiseizure” – 12,500, of which of which 3,160 have been applied in the last 5 years. The term «противоэпилептический препарат» (translation is “antiepileptic drug”) was found in 7780 works, «антиэпилептический препарат» (translation is “antiseizure drug” also) – 3910 (11,690 in total), “antiseizure drug” – 12,900 sources (in the last 5 years – 3341 and 3340, respectively). Thus, according to Google Scholar, in publications in Russian, unlike English-language sources of scientific literature, there has recently been a de facto parity in the use of the terms “antiepileptic” and “antiseizure”.
In the eLibrary database, the term «противоэпилептический» (“antiepileptic”) was contained in 1,351 publications, «противосудорожный» (“antiepileptic” also) – in 676 (2,027 in total), “antiseizure” – in 1,507 primary sources, of which in the last 5 years – in 510, 154 (664 in total) and 393 sources, respectively. The terms «противоэпилептический препарат» (“antiepileptic drug”), «антиэпилептический препарат» (“antiseizure drug” also) and “antiseizure drug” were contained in 857, 506 (1,363 in total) and 621 papers, respectively, of which 344, 122 (466 in total) and 197 in the sources of the last 5 years, respectively. According to the search query “antiepileptic”, 7661 publications were identified during the entire time of data accumulation, of which 2388 over the past 5 years, according to the search query “antiseizure” – 924 publications, of which 719 over the past 5 years. According to the search query “antiepileptic drug”, 3,572 publications were identified during the entire time of data accumulation, 1,077 of them over the past 5 years, 324 publications were identified according to the search query “antiseizure drug”, 256 of them over the past 5 years. Thus, the use of the term “antiepileptic” dominated the scientific sources of eLibrary database.
Results of the survey in epileptologists and epilepsy patients / Результаты опроса врачей-эпилептологов и больных эпилепсией
111 people took part in the survey posted on the instant messaging service Telegram, and 68 people participated in the social media platform VK. The total number of participants was 179 (Table 3). More than a half (56.42%) of the respondents spoke in favor of the traditionally used terminology “antiepileptic drugs” (AED), “antiepileptic medication”. The second most popular (18.44%) was the answer “Not differed, interchangeable terminology”. Only 17.32% of the participants preferred the terminology “antiseizure drugs/medications” (ASD/ASM), proposed by the ILAE. Another 7.82% left the answer unchallenged.
Table 3. A questionnaire survey results on public online resources of the non-profit partnership “The Association of Epileptologists and Patients”, n (%)
Таблица 3. Результаты опроса на публичных онлайн-ресурсах некоммерческого партнерства «Сообщество
врачей-эпилептологов и больных эпилепсией», n (%)
Answers / Варианты ответов | The channel in instant messaging service Telegram / Канал в мессенджере Telegram | The community in social media platform VK / Сообщество в социальной сети ВКонтакте | Total / Всего |
“Antiseizure drug” (ASD), “antiseizure medication” (ASM), “anticonvilsants”, “antiseizure therapy” / «Противосудорожные препараты» (ПСП), «противосудорожные средства» (ПСС), «противоприступные препараты» (ППП), «антиконвульсанты», «противосудорожная терапия», «противоприступная терапия» | 16 (14,41) | 15 (22,06) | 31 (17,32) |
“Antiepileptic drug” (AED), “antiepileptic medication” (AEM), “antiepileptic therapy” / «Противоэпилептические препараты» (ПЭП), «антиэпилептические препараты» (АЭП), «противоэпилептическая терапия», «антиэпилептическая терапия» | 64 (57,66) | 37 (54,41) | 101 (56,42) |
Not differed, interchangeable terminology / Разницы нет, терминология является взаимозаменяемой | 22 (19,82) | 11 (16,18) | 33 (18,44) |
Undetermined / I want to see the results of the survey // | 9 (8,11) | 5 (7,35) | 14 (7,82) |
Итого / Total | 111 (100,00) | 68 (100,00) | 179 (100,00) |
DISCUSSION / ОБСУЖДЕНИЕ
Recently there has been more and more importance attached to the terminology used to describe medicines indicating the nature of their main therapeutic effect. So, in the 1990s. a scheme of drug name systematization was introduced for mononclonal antibodies. According to the scheme, in addition to the variable prefix, the term contains a basis reflecting the target pathology (for example, pathology of the immune system – “-li(m)-”,
malignant neoplasms in the ovaries – “-go(v)-”, in the mammary gland – “-ma(r)-”, other localization – “-tu(m)-”,
etc.), and the origin of the antibody (mouse – “-o-”, chimeric – “-xi-”, humanized – “-zu-”, human – “-u-”, etc.), as well as the ending is “-mab” (eng. mab – monoclonal antibody): for example, “ada-lim-u-mab” means “human monoclonal antibody targeting the immune system” [16, 17]. Moreover, in 2021, monoclonal antibodies instead of “-mab” received four new endings: “-tug” (interacting with one epitope), “-bart” (artificially constructed), “-mig” (the antibodies with a bi- or multi-specificity) and “-ment” (fragments of antibodies) [18].
The development and introduction of drugs used for epilepsy occurred for the most part in the twentieth century, so there are no universal rules for their description and naming.
The ILAE experts noticed the fact that most medicines used in patients with epilepsy produce their effect by suppressing the symptoms (seizures) and are approved on the basis of the data on the symptomatic effect on convulsive activity. Therefore, according to the position of the ILAE, the most appropriate term for naming such drugs is the term “antiseizure medication”, and the term “antiepileptic drug” is not recommended for remedies that essentially have a symptomatic effect and only indirectly, through suppression of seizures, can positively affect the underlying disease (epilepsy) or comorbid diseases and conditions, as it can mislead epilepsy patients, their caregivers, the general public, as well as some medical professionals, by instilling belief that these drugs treat the underlying disease, and the disappearance of symptoms necessarily means a cure [1]. Noting that this issue is highly relevant for all languages, the ILAE experts call for appropriate measures to be taken to develop recommendations on adequate terminology, taking into account the specific social and cultural context and the need for broad involvement of all stakeholders – both the medical community and patients.
Russian language has been one of the global languages since the 20th century, which is enshrined by the United Nations, where Russian is one of the six official languages. By the degree of prevalence, Russian ranks 9th in the world. Although the prevalence of the Russian language in the world is decreasing due to the replacement by local languages in the countries of the former USSR and some decline in population, it is native to 130 million citizens of the Russian Federation, 26.4 million citizens of other post-Soviet countries and 7.4 million residents of other countries. In addition, more than 114 million people around the world speak Russian as a second language or know it as a foreign language [19–22].
Based on these assumptions, it seemed important to clarify application profile in the Russian language of the terms in question and to identify differences in semantics in order to understand and clarify the issue of how it is possible to adapt the recommendations of the ILAE to the Russian-speaking community. Since the analysis of the usage frequency of the terms denoting drugs used for epilepsy in real practice has not been carried out before, we have undertaken such an analysis with regard to terminology in both English and Russian. At the same time, we have identified several target groups: representatives of the general public not immersed in the context of epilepsy, i.e. who are not selected basing on the principle of having specialized education or presence of the disease; professional community of the researchers who publish scientific articles on the topic; practicing epileptologists and patients with epilepsy. The profile of the use of the terminology studied by the general public was assessed with the use of search query analysis systems in the leading Internet search engines, by professional researchers – by the number of publications in leading ISD, by practicing epileptologists and their patients – by questioning on online resources comprised by the largest public organization in Russia. This made it possible to ensure the maximum representativeness of the study.
According to the profile of search queries in Google Trends, it was found that the queries using the term “antiepileptic” on the Internet are made more than 5 times more often than the ones using the term “antiseizure”, which convincingly demonstrates its higher prevalence among the broad masses of the population using English. Since the term “antiepileptic” in Russian corresponds to two terms – «противоэпилептический» and «антиэпилептический», they were taken into account separately, and only then, the results were summarized. When analyzing search queries in Yandex Wordstat, it was revealed that the profile of the use of these terms in the Russian-speaking community differs from that in the English-speaking segment of the Internet: search for queries with the term “antiseizure” is more common here: there were almost 2.5 times more such queries than with the term “antiepileptic”.
The application profile of these terms in professional medical community is no less interesting. First of all, it is noteworthy that the scientific primary sources containing this terminology both in Pubmed /MEDLINE and in Google Scholar (even in Russian!) are an order of magnitude more than in Russian eLibrary. Apparently, eLibrary does not index as many primary sources as foreign ISD, although at least with regard to the sources in Russian, the opposite could be expected.
According to the results of PubMed/MEDLINE analysis, it turns out that, starting with the earliest works, the term "antiepileptic drug" (AED) has been used in the vast majority of cases by the scientific medical community. And only since 1979, first in some works, and then more and more the term “antiseizure drug” has been spreading. Nevertheless, as of today, according to the profile of usage among the English-speaking segment of professional medical community, the term “antiepileptic drug” continues to be several times more common than the term “antiseizure drug” (see Tables 1 and 2).
In the Russian-speaking segment of professional scientific community, the term “antiepileptic” is generally used as much (according to Google Scholar) or more often (according to eLibrary) than “antiseizure”. At the same time, the difference is not as dramatic as in the English-speaking segment. However, the practice of using this terminology by the scientific community contradicts that of the broad Russian speaking segment of population not immersed in the context, and the term “antiseizure” is more popular here. Apparently, this is due to the desire of the Russian-speaking scientific community to match the terminology of most foreign publications, as “antiepileptic drug” (AED) is most commonly used there, thus the same term has become widespread in the works of Russian-speaking authors. The influence of foreign sources on the general population is less, so they historically use a different term.
The majority of practicing epileptologists and epilepsy patients, whom we attributed to a population immersed in the context, are, for obvious reasons, more aware of etiology, pathogenesis, diagnosis, treatment approaches and prognosis than the general population, preferred terminology as “antiepileptic drugs” (AED); “antiepileptic therapy”, “antiepileptic medication” (AEM). It is particularly noteworthy that there are several more people who consider the terms “antiepileptic” and “antiseizure” interchangeable rather than those supporting the use of the term “antiseizure” (“antiseizure medications” (ASM), “anticonvulsants” (ACD), etc.). Thus, the profile of terminology used by broad masses of the population not immersed in the context had differences: while the English-speaking population used the term “antiepileptic” more frequently, the Russian-speaking population used “antiseizure” more. At the same time, the profile of the use of terminology in real practice in the Russian-speaking professional scientific community coincided with the English-speaking community, as did the assessment results in practicing epileptologists and epilepsy patients. It has been clearly demonstrated that the opinion of the ILAE experts is not shared by the representatives of either English-speaking or Russian-speaking segments.
Perhaps, it is based on the understanding that antiepileptic drugs control epilepsy, a disease that can manifest itself not only in seizures. The fact is that in the last definition of the ILAE, manifestations of epilepsy are not clearly spelled out [13, 23]. It lists unprovoked (or reflex) seizures and the diagnosis of epileptic syndrome on the criteria. Meanwhile, in some forms of epilepsy, for example, electrical status epilepticus in sleep (ESES), especially in childhood, the only noticeable manifestation may be cognitive impairment [24–26]. At focal epilepsy, with localization of an epileptogenic focus in a negative field, seizures with loss of activity are observed. Children have atonic seizures, which are an integral part of the epileptic syndrome. The ILAE experts point out that in addition to epilepsy, psychogenic seizures are often found (eg. psychogenic nonepileptic seizure, PNES), which have nothing to do with epilepsy, and their leading symptom are seizures, as well as functional dissociative seizures (FDS), i.e. convulsive seizures with motor, sensory, mental or vegetative manifestations that resemble epileptic seizures, but are not caused by epileptogenic activity [1, 27–30]. These seizures are not treated with anticonvulsants, but with a combination of antidepressants with neuroleptics and benzodiazepines. In addition, it is necessary to differentiate between cataplexy attacks and narcolepsy, with the latter, although extremely rare, there may be conditions combined with epileptic seizures. It is important to bear it in mind that we treat epilepsy, not seizures, because the seizures themselves and their combination make up the clinical picture of an epileptic syndrome or a form of epilepsy. These arguments speak in favor of a more precise definition – “antiepileptic drugs”. The introduction of the term “antiseizure” in practice can lead to confusion and their prescription is not based on indications. In addition, there the classic approach is that we treat a sick person, not the symptoms of the disease, i.e. a patient with epilepsy, not seizures.
There is no negative connotation of drugs with narcotic drugs in the Russian language, as well as the similarity of abbreviations with the abbreviations denoting autism spectrum disorders and atrial septal defect, therefore the recommendation to avoid the word “drug" is not applicable. On the contrary, the word “seizure” in the sense of “fit” in Russian («припадок») has a negative connotation: this word often refers to unacceptable behavior (“in a fit of jealousy”, “in a fit of anger”, etc.). The use of the term “seizure” may further stigmatize a patient with epilepsy, therefore it is justified to recommend the use of the terms “convilsive ictus”, “epileptic ictus” instead of “convulsive seizure”, “epileptic seizure”.
Thus, for medicines and therapeutic methods used to control epilepsy, it is preferable to continue using the synonyms “antiepileptic drugs” (AED), “antiepileptic medications” (AEM).
In the context of adaptation to the Russian language, it seems possible to reduce recommendations of the ILAE on terminology of medicines used to control convulsive disorders to the following basic provisions: the terms “antiepileptic” and “antiseizure” should not be considered as mutually exclusive to denote treatment that has a direct effect on the course of epilepsy; instead of the term “seizure”, “epileptic seizure” it is preferable to use the terms “convulsive ictus”, “epileptic ictus”.
Limitations of the study / Ограничения исследования
The strong side of this work is in its novelty as no profile of the use of epilepsy terminology and, in particular, for the drugs used to control it have not been identified in the scientific literature before. However, the limitations of the study include the use of the Internet resources as not all epilepsy patients have an access to it. Therefore, an integrated assessment using both the analysis of online resources and the results of an offline survey would be most objective. Another limitation is inability to differentiate the survey participants on the online resources of the non-profit partnership “Association of Epileptologists and Patients” into cohorts of practicing epileptologists and epilepsy patients, since there were no technical possibilities for verification.
CONCLUSION / ЗАКЛЮЧЕНИЕ
The discussion on whether drugs used in epilepsy patients to control seizures should be called “antiepileptic” or “antiseizure” reflects the changing understanding of etiology and pathogenesis of epilepsy, the mechanism of action and place in the management of such patients throughout the XX and XXI centuries. While the term “antiepileptic” emphasizes an integrated approach to the treatment of epilepsy, including seizure control and treatment of concomitant manifestations and diseases, the term “antiseizure” emphasizes the main pharmacological effect of these drugs, mainly consisting in symptomatic suppression of seizures.
In the Russian-speaking community, the terms “antiepileptic drug” (AED), continue to be more applicable than “antiseizure medication” (ASM). Ultimately, the choice of terminology may vary depending on the clinical context and changing perceptions of epilepsy as a holistic neurological disorder. It is advisable to return to the issue of improving the definition and classification of epilepsy.
1 https://ilae.org.
2 https://google.com/trends.
3 https://wordstat-2.yandex.ru.
4 https://pubmed.ncbi.nlm.nih.gov.
5 https://scholar.google.com/.
6 https://www.elibrary.ru/.
7 https://t.me/EpilepsyAssociation.
8 https://vk.com/public211196330.
References
1. Perucca E., French J.A., Aljandeel G., et al. Which terms should be used to describe medications used in the treatment of seizure disorders? An ILAE position paper. Epilepsia. 2024; 65 (3): 533–41. https://doi.org/10.1111/epi.17877.
2. Linstone H.A., Turoff M. (Eds.). The Delphi method: techniques and applications. Addison-Wesley; 1975: 3–12.
3. Wirrell E.C., Nabbout R., Scheffer I.E., et al. Methodology for classification and definition of epilepsy syndromes with list of syndromes: report of the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022; 63 (6): 1333–48. https://doi.org/10.1111/epi.17237.
4. Zuberi S.M., Wirrell E., Yozawitz E., et al. ILAE classification and definition of epilepsy syndromes with onset in neonates and infants: position statement by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022; 63 (6): 1349–97. https://doi.org/10.1111/epi.17239.
5. Riney K., Bogacz A., Somerville E., et al. International League Against Epilepsy classification and definition of epilepsy syndromes with onset at a variable age: position statement by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022; 63 (6): 1443–74. https://doi.org/10.1111/epi.17240.
6. Blinov D.V. Epilepsy syndromes: the 2022 ILAE definition and classification. Epilepsia i paroksizmal'nye sostoania / Epilepsy and Paroxysmal Conditions. 2022; 14 (2): 101–82 (in Russ.). https://doi.org/10.17749/2077-8333/epi.par.con.2022.123.
7. Tatum W.O., Mani J., Jin K., et al. Minimum standards for inpatient long-term video-EEG monitoring: a clinical practice guideline of the International League Against Epilepsy and International Federation of Clinical Neurophysiology. Clin Neurophysiol. 2022; 134: 111–28. https://doi.org/10.1016/j.clinph.2021.07.016.
8. Jafari A., Rezaei-Tavirani M., Parvareshi Hamrah M., et al. Psychogenic non-epileptic seizures; a narrative review. Arch Acad Emerg Med. 2020; 8 (1): e10.
9. Liampas A., Markoula S., Panagiotis Z., Reuber M. Psychogenic non-epileptic seizures (PNES) in the context of concurrent epilepsy – making the right diagnosis. Acta Epileptol. 2021; 3 (1): 23. https://doi.org/10.1186/s42494-021-00057-x.
10. Gaskell C., Power N., Novakova B., et al. A meta-analytic review of the effectiveness of psychological treatment of functional/dissociative seizures on non-seizure outcomes in adults. Epilepsia. 2023; 64 (7): 1722–38. https://doi.org/10.1111/epi.17626.
11. Hingray C., Ertan D., Reuber M., et al. Heterogeneity of patients with functional/dissociative seizures: three multidimensional profiles. Epilepsia. 2022; 63 (6): 1500–15. https://doi.org/10.1111/epi.17230.
12. Popkirov S., Asadi-Pooya A.A., Duncan R., et al. The aetiology of psychogenic non-epileptic seizures: risk factors and comorbidities. Epileptic Disord. 2019; 21 (6): 529–47. https://doi.org/10.1684/ epd.2019.1107.
13. Fisher R.S., van Emde Boas W., Blume W., et al. Epileptic seizures and epilepsy: definitions proposed by the international league against epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005; 46 (4): 470–2. https://doi.org/10.1111/j.00139580.2005.66104.x.
14. Lopez M.R., LaFrance W.C. Treatment of psychogenic nonepileptic seizures. Curr Neurol Neurosci Rep. 2022; 22 (8): 467–74. https://doi.org/10.1007/s11910-022-01209-3.
15. Kinglake R. On the reputed anti-epileptic power of argentum nitratum. Med Phys J. 1801; 5 (27): 435–41.
16. Recommendation of the Board of the Eurasian Economic Commission dated April 23, 2019 No. 13 “On the Rules for the preparation of group names of medicinal products”. Available at: https://www.consultant.ru/document/cons_doc_LAW_323626/ (in Russ.) (accessed 03.03.2024).
17. Principles of assigning international nonproprietary names (INN) to biological and biotechnological preparations. Clinical Microbiology and Antimicrobial Chemotherapy. 2007; 9 (2): 121–32 (in Russ.).
18. New INN monoclonal antibody (mAb) nomenclature scheme. World Health Organization. 2021. Available at: https://cdn.who.int/media/docs/default-source/international-nonproprietary-names-(inn)/new_mab_-nomenclature-_2021.pdf (accessed 03.03.2024).
19. What are the top 200 most spoken languages? Ethnologue. 2024. Available at: https://www.ethnologue.com/insights/ethnologue200/ (accessed 03.03.2024).
20. Arefyev A. How many people speak and will speak Russian? Demoscope. 2006; 251–252 (in Russ.). Available at: https://www.emoscope.ru/weekly/2006/0251/tema04.php (accessed 03.03.2024).
21. Gavrilov K., Kozievskaya E., Yatsenko E. Is Russian a Soviet language? Demoscope. 2008; 329–330 (in Russ.). Available at: https://www.demoscope.ru/weekly/2008/0329/tema01.php (accessed 03.03.2024).
22. Gavrilov K., Kozievskaya E., Yatsenko E. Where there is a need to learn Russian. Demoscope. 2008; 329–330 (in Russ.). Available at: https://www.demoscope.ru/weekly/2008/0329/tema04.php (accessed 03.03.2024).
23. Fisher R.S., Acevedo C., Arzimanoglou A., et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014; 55 (4): 475–82. https://doi.org/10.1111/epi.12550.
24. Kholin A.A. Epileptic encephalopathies with electrical status epilepticus of slow-wave sleep (ESES): diagnosis and pharmacotherapy. Epilepsia i paroksizmal'nye sostoania / Epilepsy and Paroxysmal Conditions. 2018; 10 (1): 63–71 (in Russ.). https://doi.org/10.17749/2077-8333.2018.10.1.063-071.
25. Posar A., Visconti P. Cognitive deterioration in childhood: never forget electrical status epilepticus during slow-wave sleep. Brain Circ. 2023; 9 (1): 48–9. https://doi.org/10.4103/bc.bc_49_22.
26. Lu G., Cheng Y., Wang Y., et al. The prevalence and risk factors of electrical status epilepticus during slow-wave sleep in self-limited epilepsy with centrotemporal spikes. Clin EEG Neurosci. 2024; 55 (2): 265–71. https://doi.org/10.1177/15500594231182758.
27. Sobregrau P., Baillès E., Carreño M., et al. Psychiatric and psychological assessment of patients with drug-resistant epilepsy and psychogenic nonepileptic seizures (PNES) with no response to previous treatments. Epilepsy Behav. 2023; 145: 109329. https://doi.org/10.1016/j.yebeh.2023.109329.
28. Reilly C., Jette N., Johnson E.C., et al. Scoping review and expertbased consensus recommendations for assessment and management of psychogenic non-epileptic (functional) seizures (PNES) in children: a report from the Pediatric Psychiatric Issues Task Force of the International League Against Epilepsy. Epilepsia. 2023; 64: 3160–95. https://doi.org/10.1111/epi.17768.
29. Hassan J., Taib S., Yrondi A. Structural and functional changes associated with functional/dissociative seizures: a review of the literature. Epilepsy Behav. 2024; 152: 109654. https://doi.org/10.1016/j.yebeh.2024.109654.
30. Gaskell C., Power N., Novakova B., et al. A meta-analytic evaluation of the effectiveness and durability of psychotherapy for adults presenting with functional dissociative seizures. Seizure. 2024; 119: 98–109. https://doi.org/10.1016/j.seizure.2024.05.016.
About the Authors
D. V. BlinovRussian Federation
Dmitry V. Blinov, PhD, MBA
4/10 Sadovaya-Triumfalnaya Str., Moscow 127006
5 bldg 1-1a 2nd Brestskaya Str., Moscow 123056
37А bldg 1 Altufyevskoe Shosse, Moscow 127410
WoS ResearcherID: E-8906-2017. Scopus Author ID: 6701744871
A. S. Petrukhin
Russian Federation
Andrey S. Petrukhin, Dr. Sci. Med., Prof.
1 Ostrovityanov Str., Moscow 117513
Scopus Author ID: 7005313493
K. V. Voronkova
Russian Federation
Kira V. Voronkova, Dr. Sci. Med., Prof.
1 Ostrovityanov Str., Moscow 117513
1a Litovskiy blvd, Moscow 117593
Scopus Author ID: 20434946200
E. S. Akarachkova
Russian Federation
Elena S. Akarachkova, Dr. Sci. Med.
40 Musa Dzhalil Str., Moscow 115573
Scopus Author ID: 23048541100
O. V. Kotova
Russian Federation
Olga V. Kotova, PhD, Assoc. Prof.
6 Miklukho-Maklay Str., Moscow 17198
A. N. Mnatsakanyan
Russian Federation
Anna N. Mnatsakanyan, PhD, Assoc. Prof.
5 bldg 1 2nd Baumanskaya Str., Moscow 105005
G. P. Kurchatkina
Russian Federation
Galina P. Kurchatkina
5 bldg 1 2nd Baumanskaya Str., Moscow 105005
Review
For citations:
Blinov D.V., Petrukhin A.S., Voronkova K.V., Akarachkova E.S., Kotova O.V., Mnatsakanyan A.N., Kurchatkina G.P. Terminology of medicines used to control seizure disorders: 2024 ILAE Recommendations and profile of real-world term use. Epilepsy and paroxysmal conditions. 2024;16(3):176–191. https://doi.org/10.17749/2077-8333/epi.par.con.2024.209
JATS XML

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.










































