Scroll to:
“Between Scylla and Charybdis”: the influence of pregravid preparation on mental development of children born to mothers with epilepsy
https://doi.org/10.17749/2077-8333/epi.par.con.2024.191
Abstract
Background. The emergence of the latest pharmacotherapeutic methods opened up new opportunities for delivery of healthy children born to women with epilepsy, whereas comprehensive pregravid preparation became the “gold standard” of treatment, reducing the risks of teratogenesis and the appearance of mental development disorders and adaptation in offspring.
Objective: to study an effect of a comprehensive pregravid preparation for women with epilepsy on mental development and adaptation in paired children.
Material and methods. A multicenter, retrospective, uncontrolled, open, observational study assessing mental development level in children born to women with epilepsy was conducted. The study involved 176 subjects: 88 children (aged 3–9 years) and paired mothers with epilepsy. Several methods we used: a medical questionnaire (biographical data, clinical data on the form, course and treatment of maternal epilepsy, course of pregnancy and childbirth, as well as information on pediatric early development), Luria neuropsychological batteries adapted by J.M. Glozman (for preschool and primary school children), Wechsler Intelligence Scale for Children (WISC) (for children aged 5 years and older), Child Behavior Checklist (CBCL) forms for parents (by T. Achenbach), and attention deficit hyperactivity disorder and other behavioral dysfunctions questionnaire modified by N.N. Zavadenko (for children aged 5 years and older).
Results. In children born to mothers who did not undergo pregravid preparation, the overall indicator of developmental and adaptation disorders was higher: anxiety, attention problems, motor awkwardness, hyperactivity and internalization problems were more pronounced. They also had a higher overall index of neuropsychological disorders – gnosis, phonemic hearing, understanding of reversed speech and speech logic, and logical operations were specifically affected. A comparison of age groups showed that by the age of 7–9 years old, children born to mothers who underwent pregravid preparation were better compensated. Seizures during pregnancy is a predictor for developing large number of pediatric mental development disorders in the future (somatic problems, disorders of socialization and attention, motor awkwardness, externalization problems), whereas conducting pregravid preparation significantly lowers the predictive power of such effect, which allows to consider it as a moderator. Pregravid preparation is also a moderator that lowers a negative impact of toxicosis on probability for deliver a child with externalization (aggression) and delayed neurodynamic development.
Conclusion. A comprehensive pregravid preparation exhibits a moderating effect: it lowers a negative impact of epileptic seizures and pregnancy complications (toxicosis) on further mental development and adaptation of children, as well as increases their compensatory capabilities. The study results have both scientific and significance for neurologists, obstetricians as well as gynecologists and clinical psychologists.
Keywords
For citations:
Krasko A.S., Mikhailova N.F., Larina I.V., Mikhailov V.A., Odintsova G.V. “Between Scylla and Charybdis”: the influence of pregravid preparation on mental development of children born to mothers with epilepsy. Epilepsy and paroxysmal conditions. 2024;16(4):298-315. https://doi.org/10.17749/2077-8333/epi.par.con.2024.191
INTRODUCTION / ВВЕДЕНИЕ
Pregravid preparation (preparation for pregnancy) is an essential component for strengthening the health of a mother and a child. Rationally planned pregravid preparation notably lowers a risk of delivering children with congenital malformations caused by micronutrient deficiency and unrelated to hereditary defects [1].
International registries of pregnancies with epilepsy replenish the lack of studies unable to conduct international clinical trials with new antiepileptic drugs (AEDs) in pregnant women due to ethical restrictions [2]. At the same time, pregnancy with epilepsy exhibits specific characteristics such as a risk of worsening disease course during pregnancy (uncontrolled seizures), higher frequency of multiple pregnancy complications (toxicosis, anemia, gestosis, etc.), as well as the potential AED-related fetal adverse effects (teratogenesis) [3].
For patients with epilepsy, it is especially important to plan pregnancy before conception so that the most effective and safe antiepileptic treatment protocol, in which the expected therapeutic benefit would exceed potential teratogenesis risks associated with drug use is selected [4].
Thus, a neurologist who accompanies pregnancy with epilepsy, like Odysseus, must pass “between Scylla and Charybdis.” On the one hand, in order to avoid the risk of fetal teratogenesis, it is necessary to apply AEDs at minimum dosage and control drug concentration in the blood or replace a AED with a less toxic counterpart. On the other hand, it is important to prevent recurrence of seizures (primarily generalized convulsive seizures), which is achieved by constant therapeutic drug monitoring [4][5].
Pregravid preparation for women with epilepsy should be comprehensive including gynecological and somatic along with epileptological preparation. The main goal of epileptological preparation is to prevent seizures and reduce teratogenesis risk in a child [6]. Optimal therapy of epilepsy before conception involves monotherapy with a best efficacy/teratogenesis ratio drug [7] and folic acid (up to 13 weeks) [4].
Comprehensive pregravid preparation lowers both the risks of congenital malformations and the likelihood of neurobehavioral teratogenicity, i.e., a negative impact on pediatric neuropsychiatric development [8].
Until recently, research on AEDs-related teratogenesis in female epilepsy was mainly focused on assessing congenital physical abnormalities in offspring [9]. Studies examining the AEDs effect of on child’s mental development as well as an opportunity to correct it at the stage of pre-pregnancy training are evidently insufficient [10][11].
Pregnancy complications, increased frequency of maternal epileptic seizures related to AEDs during pregnancy are considered as risk factors and causes of neurobehavioral teratogenesis. For example, taking valproic acid during pregnancy can lead to the formation of both congenital anomalies and delayed nervous system development [12].
According to recent studies, the change in the AEDs spectrum used during pregnancy has affected not only the incidence of congenital malformations, but also improved the indicators of neuropsychic development of children born to mothers with epilepsy [13][14]. However, most studies continue to focus on the management of ongoing pregnancy, while the issues of preparing a woman with epilepsy for pregnancy remain insufficiently investigated. At the same time, the percentage of unplanned pregnancies in epilepsy remains high [2].
Therefore, assessing an impact of pregravid preparation on child's postnatal development remains relevant both in practical and scientific terms.
Objective: to study an effect of a comprehensive pregravid preparation for women with epilepsy on mental development and adaptation in paired children.
MATERIAL AND METHODS / МАТЕРИАЛ И МЕТОДЫ
Study design / Дизайн исследования
A multicenter retrospective uncontrolled open observational study analyzing level of mental development in children born to women with epilepsy was conducted to assess an impact of pregravidar preparation of mothers with epilepsy on further mental development in paired children.
Diagnostics / Диагностика
The clinical diagnosis of women with epilepsy was carried out by neurologists at the Russian Polenov Neurosurgical Institute (branch of Almazov National Medical Research Center), the City Epileptology Center of Saint Petersburg, Bekhterev National Medical Research Center for Psychiatry and Neurology and included the anamnesis (estimated disease duration, age of onset, frequency of seizures, antiepileptic therapy in anamnesis and in pregnancy, dynamics of epilepsy clinical manifestations during pregnancy). Medical data related to pregnancy, childbirth, newborn physical development and early psychomotor development were also collected.
The assessment of the child's mental and intellectual development, as well as adaptation, was carried out by psychologists from the Chair of Developmental and Differential Psychology of Saint Petersburg State University.
Cohort characteristics / Характеристика когорты
There were enrolled 176 subjects: 88 children aged 3–9 years and paired 88 mothers suffering from epilepsy.
To assess an impact of pregravid preparation on further child's mental development, the cohort was divided into 2 groups: group 1 (42 subjects) consisted of children whose birth was planned and prepared, group 2 (46 subjects) included children born to women with unprepared pregnancy. The study included children from three age groups, divided according to the methods we used and statistical expediency: 31 children aged 3–4 years, 29 children aged 5–6 years and 28 children aged 7–9 years.
Inclusion criteria:
– age of children ranging from 3 to 9 years;
– verified diagnosis of maternal epilepsy before pregnancy;
– mother's informed consent to participate in the study;
– informed consent of the child's parents to participate in the study.
Exclusion criteria:
– age of children under 3 and over 10 years old;
– mental retardation;
– parents' refusal to participate in the study.
Mothers / Матери
Age of epilepsy onset, disease duration, forms and activity
The experience of epilepsy ranged from 5 to 44 years and averaged 19 years. The age of epilepsy onset is spanned from 0 to 37 years (on average 15 years). According to the epilepsy classification by the International League Against Epilepsy [15], 44 patients (50%) had generalized epilepsy, 44 (50%) – focal epilepsy. Sixty-three mothers (72%) were in disease remission, most of them having no seizures for more than 1 year before the onset of pregnancy, and rare epileptic seizures found in the remaining subjects.
Antiepileptic therapy
At the time of delivery, 11 mothers (13%) did not take AEDs, 62 (70%) and 15 (17%) receiving monotherapy and polytherapy, respectively. The latter received first (old)-, new- and newest-generation AEDs (30 (40%) and 45 (60%) mothers, respectively).
Maternal age and pregnancy complications
The average age of a women was 28 years, ranging from 18 to 41 years that matched between groups (prepared and unprepared pregnancy). 58 (65%) mothers had pregnancy without toxicosis, with the remaining of them showing complications such as toxicosis of the first half of pregnancy, manifestations of toxicosis of the second half of pregnancy (edema, increased blood pressure, protein in urine), anemia, exacerbation of chronic diseases (pyelonephritis, cholecystitis, etc.).
Terms and routes of delivery
The gestation period at delivery ranged from 35 to 42 weeks. Most babies were born full-term after 37 weeks. Prematurity was noted in 7 cases of premature birth in accordance with the classification of degrees of prematurity [16]. 43 (49%) and 45 (51%) women gave birth to a child naturally and by Caesarean section, respectively.
Pregravid preparation
A three-layered pregravid preperation included: epileptological, gynecological and somatic preperation. Antiepileptic therapy was optimized, hormonal disorders, somatic health, vitamin and micronutrient deficiencies were corrected, including folic acid intake at least 3 months before pregnancy and throughout the first trimester (up to 12 weeks of pregnancy inclusive).
Children / Дети
The study examined 39 girls and 49 boys aged 3 years 1 month to 9 years 9 months (the average age was 5 years 5 months). All children attended pre-school educational institutions or school.
The birth body weight of the children was within the range of 1900–4500 g. In the first year of life, 32 (36%) children were artificially fed, 56 (64%) – breastfed.
Methods / Методики
The following methods were used in the study:
– a medical questionnaire describing biographical data, clinical data on the form, course and treatment of maternal epilepsy, the course of pregnancy and delivery, as well as information about early child’s development;
– to assess the level of child’s mental development and adaptation, forms for parents were used as follows: Child Behavior Checklist (CBCL) by T. Achenbach1 and a questionnaire to identify symptoms of attention deficit hyperactivity disorder (ADHD) and other behavioral disorders modified by N.N. Zavadenko (for children of at least 5 years old).
The following experimental psychological methods were used to assess child’s mental and intellectual development:
for mental development – two Luria’s batteries of neuropsychological tests adapted by J.M. Glozman (for children of 3–6 years and 7–12 years old);
for intellectual development – D. Wechsler Intelligence Scale for Children (WISC) (for children of at least 5 years old).
All methods are standardized for different paediatric age groups.
Statistic analysis / Статистический анализ
Statistical data processing was carried out using SPSS-23 (IBM, USA) software by applying nonparametric U Mann–Whitney criterion, two-factor analysis of variance (ANOVA), correlation, regression analysis and moderator analysis.
RESULTS AND DISCUSSION / РЕЗУЛЬТАТЫ И ОБСУЖДЕНИЕ
Overall disorder indicators / Общие показатели нарушений
Differences in the severity of mental development and adaptation disorders were found between groups of children born to mothers with/without pregravid preparation (Table 1). In children born after unprepared pregnancy, the overall disorder indicator was higher particularly being generally more pronounced for anxiety, attention problems, motor awkwardness, hyperactivity and internalization problems (fears, obsessions, etc.).
Table 1. Disorders of mental development, abilities and intelligence in children depending on maternal pregnancy preparedness
Таблица 1. Нарушения психического развития, способностей и интеллекта у детей в зависимости от подготовленности матери к беременности
Developmental parameters / | Unprepared pregnancy (mean rank) /Неподготовленная беременность (средний ранг) | Prepared pregnancy (mean rank) / Подготовленная беременность (средний ранг) | p (Mann–Whitney U test value) / Значимость U-критерия Манна–Уитни р |
Mental development disorders (CBCL) / Нарушения психического развития (CBCL) | n=46 | n=42 | |
Anxiety / Тревожность | 49,09 | 39,52 | 0,079 (tend/тенд) |
Attention problems / Проблемы внимания | 49,83 | 38,67 | 0,040* |
Internalization problems / Интернализационные проблемы | 49,32 | 39,23 | 0,064 (tend/тенд) |
Overall problem indicator / Общий показатель проблем | 49,20 | 39,36 | 0,071 (tend/тенд) |
Abilities and mental development (ADHD and behavioral dysfunctions questionnaire) / Способности и психическое развитие (анкета СДВГ и поведенческих расстройств) | n=31 | n=22 | |
Motor awkwardness / Моторная неловкость | 31,83 | 22,67 | 0,032* |
Hyperactivity / Гиперактивность | 31,05 | 23,76 | 0,094 (tend/тенд) |
Neuropsychological tests / Нейропсихологические пробы | |||
General characteristics – orientation / Общая характеристика – ориентировка (n=45/41) | 46,80 | 39,88 | 0,071 (tend/тенд) |
General characteristics – overall indicator (orientation, adequacy, criticality) / Общая характеристика – суммарный показатель (ориентировка, критичность, адекватность) (n=45/42) | 48,07 | 39,64 | 0,084 (tend/тенд) |
Gnosis – overall indicator / Гнозис – суммарный показатель (n=45/41) | 47,54 | 39,06 | 0,081 (tend/тенд) |
Understanding of addressed speech / Понимание обращенной речи (n=44/42) | 46,36 | 40,50 | 0,014* |
Phonematic hearing / Фонематический слух (n=18/7) | 14,56 | 9,00 | 0,097 (tend/тенд) |
Speech – understanding logic / Речь – понимание логики (n=31/26) | 32,18 | 25,71 | 0,036* |
Intelligence – exclusion of concepts / Интеллект – исключение понятий (n=40/40) | 44,98 | 36,03 | 0,026* |
Intelligence – overall indicator / Интеллект – суммарный показатель (n=40/39) | 45,24 | 34,63 | 0,022* |
Overall disorder indicator / Общий показатель нарушений (n=45/42) | 49,87 | 37,71 | 0,024* |
Intellectual subtests (WISC) / Интеллектуальные субтесты (WISC) | n=31 | n=22 | |
Arithmetic / Арифметический | 21,90 | 32,77 | 0,010* |
Missing details / Недостающие детали | 23,20 | 31,96 | 0,039* |
Encryption / Шифровка | 22,98 | 29,98 | 0,095 (tend/тенд) |
Note. * Statistically significant differences at the level of p≤0.05; "tend" – differences found at the level of statistical trend (p<0.10).
The number of children for neuropsychological tests is shown in brackets (unprepared pregnancy / prepared pregnancy) due to the testing specifics: a unique set of tools is applied for each age groups while conducting neuropsychological diagnostics – the older a child, the more tests are available allowing to compare mean indicators regardless of age (in this regard, the number of participants assessed in each individual test differs in study groups). The data highlighted in bold indicate a greater degree of mental development disorders, a greater number of errors while performing neuropsychological tests, and worse performance in intellectual subtests. CBCL – Child Behavior Checklist; ADHD – attention deficit and hyperactivity disorder; WISC – Wechsler Intelligence Scale for Children.
Примечание. * Статистически значимые различия на уровне p≤0,05; «тенд» – различия, обнаруженные на уровне статистической тенденции (p<0,10).
Для нейропсихологических проб количество детей указано в скобках (неподготовленная беременность / подготовленная беременность) в связи с особенностями тестирования: при проведении нейропсихологической диагностики для каждого возраста подбирается уникальный набор инструментов – чем старше ребенок, тем больше тестов для него доступно, при этом возможно сравнить усредненные показатели вне зависимости от возраста (поэтому группы различны по количеству участников в каждом отдельном тесте). Выделенные полужирным шрифтом данные свидетельствуют о большей степени выраженности нарушений психического развития, большем количестве ошибок при выполнении нейропсихологических проб и худшем выполнении интеллектуальных субтестов. CBCL (англ. Child Behavior Checklist) – Контрольный лист поведения ребенка; СДВГ – синдром дефицита внимания и гиперактивности; WISC (англ. Wechsler Intelligence Scale for Children) – методика исследования интеллекта Д. Векслера.
Moreover, they had also higher overall disorder rate for all neuropsychological tests compared with those born to mothers after pregravid preparation showing affected gnosis, phonemic hearing, understanding of reversed speech and speech logic. In addition, during examination situation, they were less oriented2, less adequate3 and critical4, so that such difficulties peaked while performing intellectual tests in general, especially logical operations (exclusion of concepts). Similar problems were found during subtests of WISC methodology. Difficulties in performing “Encryption” indicate insufficient volume and distribution of attention, poor coordination of movements and the speed of new skills formation. Errors in the performance of the “Missing details” subtest indicate deficiencies in visual perception and attention concentration, whereas the “Arithmetic” subtest points at the lack of concentration of arbitrary attention, insufficient intelligence and clarity in operating numerical material.
Thus, the revealed differences suggest that the children born to mothers whose pregnancy was accompanied by optimization of antiepileptic treatment and prevention of pregnancy pathology showed fewer problems in further development and adaptation.
Correlation analysis / Корреляционный анализ
The results of the correlation analysis also confirmed the importance of preparing mothers suffering from epilepsy for a childbirth (Fig. 1). Negative correlations were found between pregravid preparation and the severity of the following developmental disorders in children:
– motor awkwardness and attention problems were less pronounced in children born to mothers underwent pregravid preparation.
– they made fewer mistakes while performing intellectual tests, speech tests (for understanding reversed speech, grammar and logic of speech), operated better with numerical material (“Arithmetic” subtest) and had more developed phonemic hearing.
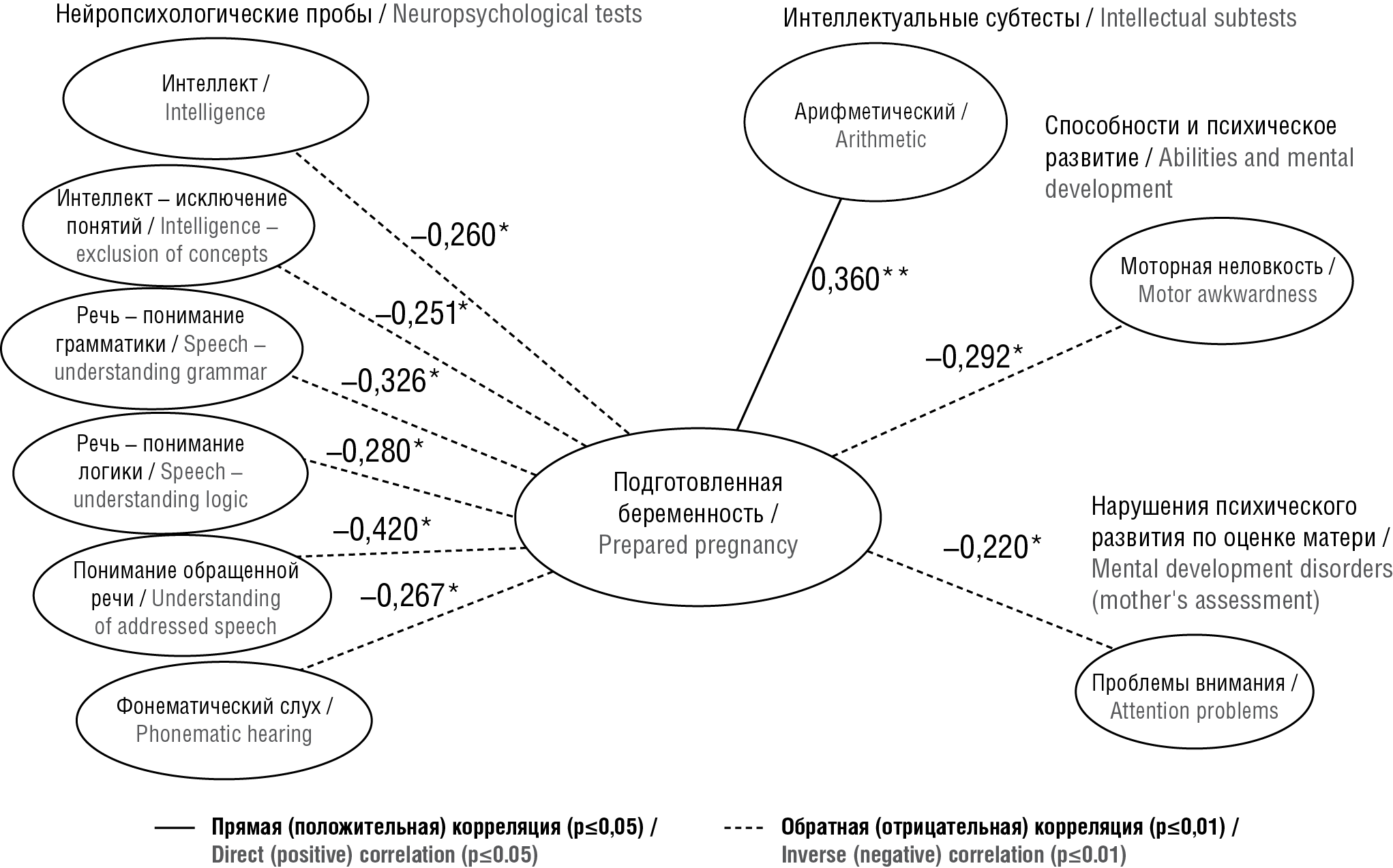
Figure 1. Correlations between mental development disorders in children and pregnancy preparedness in women with epilepsy
Рисунок 1. Корреляции между нарушениями психического развития детей и подготовленностью к беременности женщин с эпилепсией
Two-factor analysis of variance / Двухфакторный дисперсионный анализ
We assumed that the preparedness to delivery in women with epilepsy is essential for child's mental development not only in the short term, but also in the long term – i.e., to some extent, it is one of the compensation factors for disorders of child's mental development, if they were observed in an earlier developmental period.
To assess the long-term effects of pregravid preparation on child's mental development, a two-factor analysis of variance was conducted, taking into account the influence of two factors simultaneously – a child age and pregravid preparation. We were interested as to how compensation for developmental disorders occurred at similar age in children who were born to paired mothers with/without pregravid preparation. For this purpose, it was necessary to make micro-age sections and, accordingly, to stratify children from prepared and unprepared pregnancy cohorts into three age groups (3–4 years, 5–6 years and 7–9 years). Conducting two-factor analysis of variance, the study data were obtained with a high level of statistical significance.
The age dynamics related to the severity of mental health and adaptation disorders in children is presented in plots (Fig. 2) highlighted by the “multidirectional dynamics” for development and compensation disorders found in most cases. At early age (3–4 years), children from unprepared pregnancy group had more pronounced disorders symptoms, but at the same time these two groups do not differ so significantly between each other. However, by the age of 5–6, they seem to reverse places: children born to mothers undergone pregravid preparation, on the contrary, show more pronounced symptoms, but as early as at primary school age (7–9 years) had sharply decreased severity of disorders symptoms suggesting about compensation for the defect and equalization of developmentally delayed mental functions.
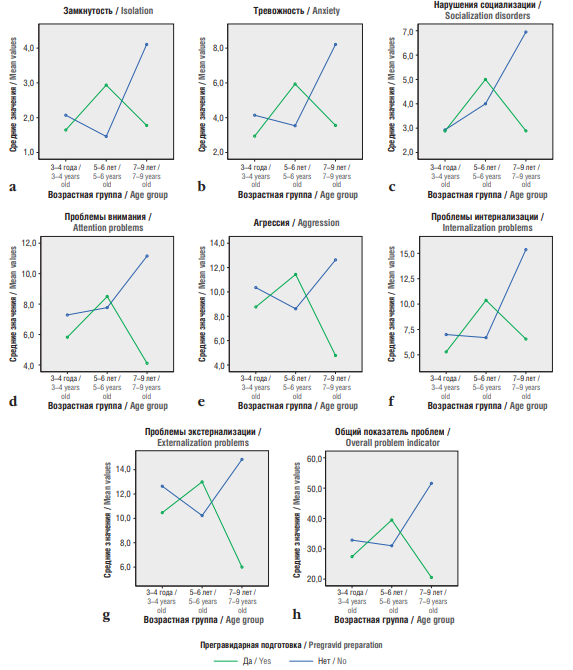
Figure 2. Age dynamics for severity of mental development and adaptation disorders in children depending on pregravid preparation for mothers with epilepsy:
a – isolation; b – anxiety; c – socialization disorders; d – attention problems; e – aggression; f – internalization problems; g – externalization problems; h – overall problem indicator
Рисунок 2. Возрастная динамика выраженности нарушений психического развития и адаптации у детей в зависимости от проведения матерям с эпилепсией прегравидарной подготовки:
а – замкнутость; b – тревожность; c – нарушения социализации; d – проблемы внимания; e – агрессия; f – проблемы интернализации; g – проблемы экстернализации; h – общий показатель проблем
At the same time, at this age (7–9 years), the children born to mothers without prior pregravid preparation showed greater isolation (p=0.019) and anxiety (p=0.015) level, more pronounced attention problems (p=0.026), aggression (p=0.015) and socialization disorders (p=0.017). They were also characterized by higher severity rate for internalization problems (fears, anxiety, isolation, etc.) (p=0.007), externalization (delinquent, aggressive behavior, oppositional defiant behavior) (p=0.031), as well as greater overall problems indicator (p=0.006).
A similar dynamic pattern in developing mental functions is observed in premature infants, and has been called the “false start” phenomenon described by S. Blüml et al. [17] and confirmed in the study by N.I. Bakushkina and E.R. Isaeva [18].
S. Blüml et al. examining premature vs. full-term infants lacking any brain injuries showed that the process of synchronization of maturation for brain white and gray matter is disrupted. It has been found that physiological changes and/or stimulating factors can trigger the premature or “false” onset of specific developmental events. The authors suggested to call this phenomenon a “false start” implying a profoundly increased biochemical processes determining brain white matter maturation followed by an abnormal decline (relative to the normal trajectory) in intensity of such processes. That is, the function begins to emerge even before it is ready for development. This process is mainly observed in brain white matter. The authors prove that even in infants “with unremarkable MRI scans” the biochemical profile of key metabolites associated with axon development, energy metabolism and membrane generation becomes changed. Hence, even in infants in whom magnetic resonance imaging reveal no external signs of abnormality, such data suggest that the cellular processes supporting brain development can be altered [17].
In addition, it was shown that prematurity had none/little effect on metabolic processes in the brain. Early birth only affected some metabolites in the white matter presumably suggesting that it also acts on the timing and synchronization of developmental processes. O. Kapellou et al. emphasize that “prematurity does not damage the cerebral cortex in isolation, but disrupts the coordinated growth of the entire brain” [19].
The peak synaptogenesis begins at 34 weeks and continues in the early postnatal period [20]. Its dynamics differ at individual measurement points in various cortical areas both in infancy and older age [20][21].
N.I. Bakushkina and E.P. Isaeva [18] conducted a longitudinal study and identified special trajectories for development of cognitive functions influenced by periods of synaptogenesis in the primary sensory and prefrontal cortex observed in premature vs. full-term infants aged 3 months to 3 years. It has been proven that these trajectories are influenced by periods of synaptogenesis – phases (during the period of maximum synapse formation or post-peak state) occurring in those brain areas that are responsible for relevant functions. Premature infants demonstrate normal development during peak synaptogenesis, whereas in post-peak periods – lower rates of cognitive development, receptive communication, and development of fine and large motor skills compared with full-term infants. Differences in neurocognitive development in most premature infants are leveled without any intervention: by the age of 14 months – for receptive communication and large motor skills, by 24 months – for fine motor skills [18].
We suggest that a similar effect may be observed in children born to mothers with epilepsy, as a long-term result of AED-related teratogenic effect on child’s neurocognitive development because synaptogenesis processes occur not only early, but also at later age. This is evidenced by uneven mental development, which proceeds differently at similar age in children born to mothers after prepared and unprepared pregnancy. Moreover, it underlies the dynamic development of both a set of mental functions as “prerequisites of intelligence” (gnosis, praxis, neurodynamics), and its more integrated structures particularly speech and intelligence.
Whereas at early age, differences between these two groups of children are observed in developing basic mental functions, then by the age of 7–9, differences in social and psychological functioning (problems of socialization, internalization, externalization, etc.) become apparent – i.e., “secondary” social adaptation disorders.
We obtained similar results while using the clinical scale for detecting symptoms of ADHD and other behavioral disorders modified by N.N. Zavadenko (Fig. 3). By the age of 7–9, children born to mother after unprepared pregnancy showed more marked cerebrastenic symptoms, psychosomatic disorders, fears, impaired oral speech, attention deficit, emotional-volitional disorders, behavior problems, oppositional and aggressive reactions.
We found similar dynamics while assessing the level of mental development in children using neuropsychological methods. But if in the first two cases the mothers self-assessed the mental development and adaptation of paired children by using CBCL and a questionnaire to identify symptoms of ADHD and other behavioral disorders (modified by N.N. Zavadenko), then in this case the Wexler test and neuropsychological data are considered an objective assessment.
We found that by the age of 7–9 years, children born to paired mothers not underwent pregravid preparation were less compensated than those children born after prepared pregnancy. Despite that after unprepared pregnancy children in the older preschool age coped well enough with tasks, at primary school age they lagged behind in the development of basic mental functions, which are traditionally considered “prerequisites of intelligence”.
Firstly, children born to mothers without pregravid preparation were less oriented and behaved less adequately in the examination situation (Fig. 4). Secondly, they lagged behind in the development of general gnosis particularly subject (naming of objects) and spatial (spatially oriented figures) gnosis (Fig. 5). In addition, the level of speech development was generally better in children born to mothers underwent pregravid preparation (Fig. 6).
Despite that at early age (3–4 years old), children after unprepared pregnancy made much more mistakes in logical tests (isolating the meaning of plot pictures), nevertheless, by preschool (5–6 years old) and primary school age (7–9 years old) they were able to compensate for and almost did not differ from each other (Fig. 7).
Thus, the results of two-factor analysis of variance showed that severe problems of mental development and adaptation were observed as early as at the age of 3–4 years old in both groups, however, compensatory capabilities were better in children born to mothers undergone pregravid preparation. It suggests that children in both groups were affected by AEDs, but in prepared pregnancy group, pregravid preparation helped to ameliorate such an affect and enhance compensatory reserve5.
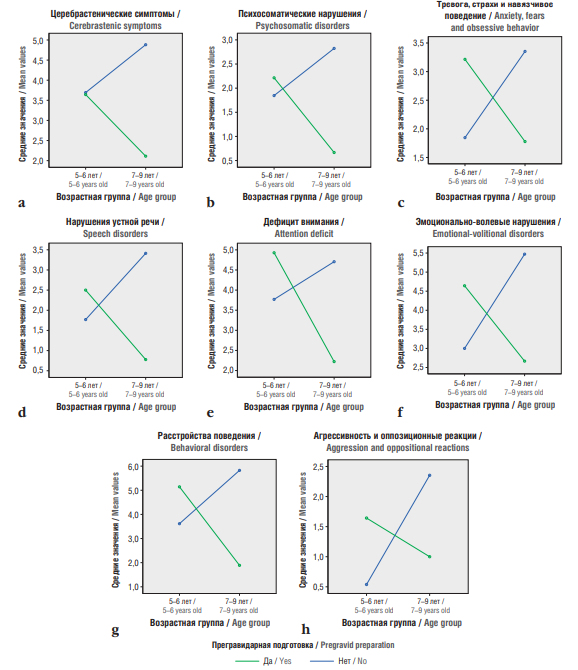
Figure 3. Age dynamics in attention deficit hyperactivity disorder and other behavioral disorder symptoms in children depending on pregravid preparation for mothers with epilepsy:
a – cerebrastenic symptoms; b – psychosomatic disorders; c – anxiety, fears and obsessive behavior; d – speech disorders; e – attention deficit; f – emotional-volitional disorders; g – behavioral disorders; h – aggression and oppositional reactions
Рисунок 3. Возрастная динамика симптомов синдрома дефицита внимания и гиперактивности и других поведенческих расстройств у детей в зависимости от проведения матерям с эпилепсией прегравидарной подготовки:
а – церебрастенические симптомы; b – психосоматические нарушения; c – тревога, страхи и навязчивое поведение; d – нарушения устной речи; e – дефицит внимания; f – эмоционально-волевые нарушения; g – расстройства поведения; h – агрессивность и оппозиционные реакции
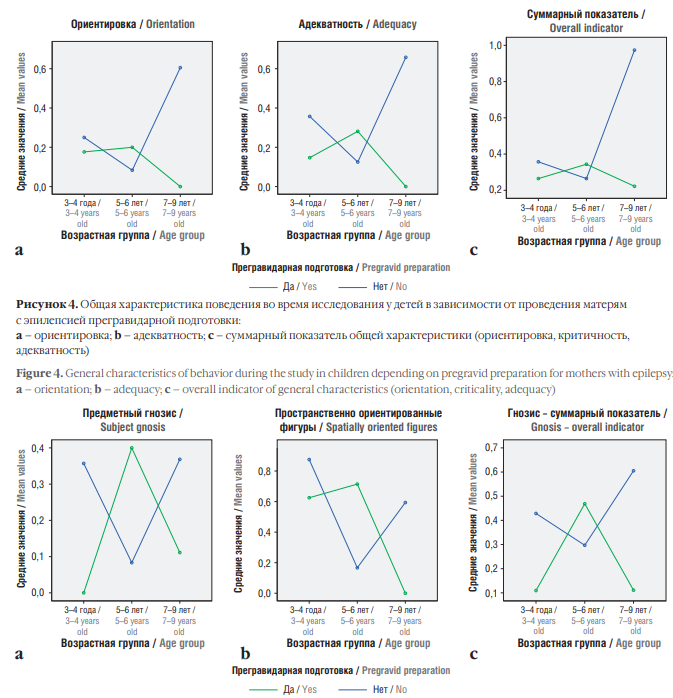
Figure 4. General characteristics of behavior during the study in children depending on pregravid preparation for mothers with epilepsy:
a – orientation; b – adequacy; c – overall indicator of general characteristics (orientation, сriticality, adequacy)
Рисунок 4. Общая характеристика поведения во время исследования у детей в зависимости от проведения матерям с эпилепсией прегравидарной подготовки:
а – ориентировка; b – адекватность; c – суммарный показатель общей характеристики (ориентировка, критичность, адекватность)
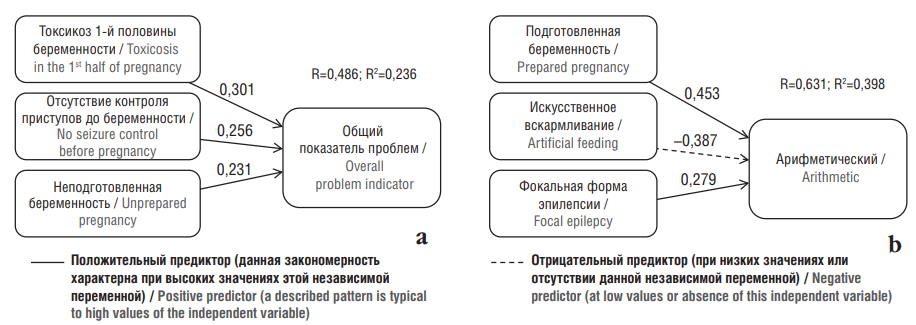
Figure 5. Dynamics of gnosis development in children depending on pregravid preparation for mothers with epilepsy:
a – subject gnosis; b – spatially oriented figures; c – overall indicator of gnosis development
Рисунок 5. Динамика развития гнозиса у детей в зависимости от проведения матерям с эпилепсией прегравидарной подготовки:
a – предметный гнозис; b – пространственно ориентированные фигуры; c – суммарный показатель развития гнозиса
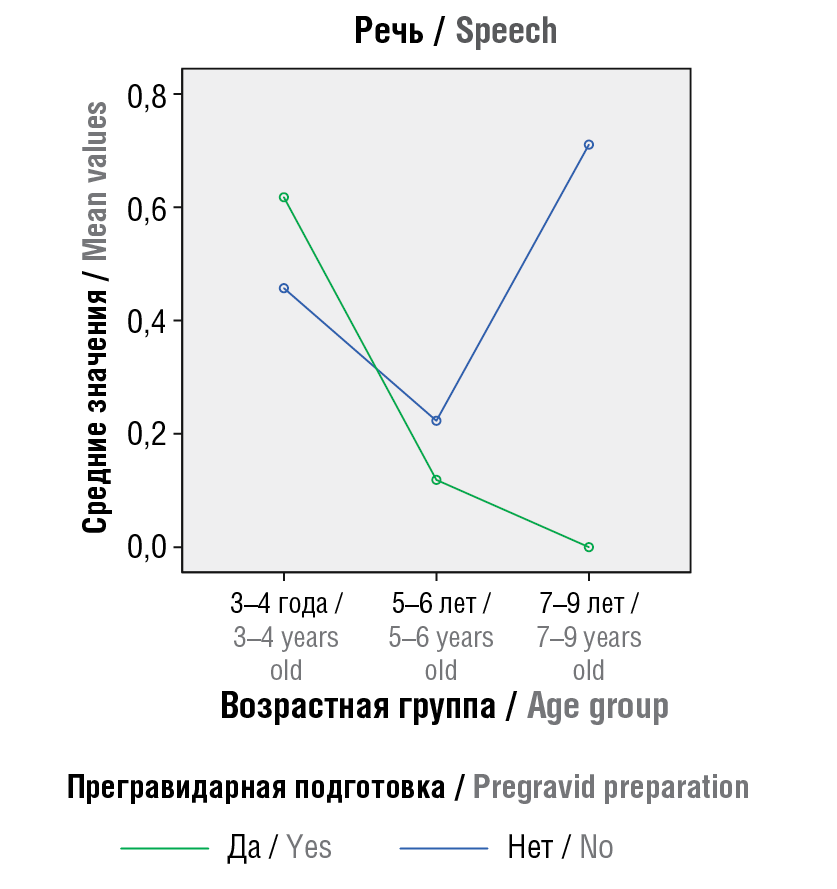
Figure 6. The level of speech development in children (overall indicator) depending on pregravid preparation for mothers with epilepsy
Рисунок 6. Уровень развития речи у детей (суммарный показатель) в зависимости от проведения матерям с эпилепсией прегравидарной подготовки
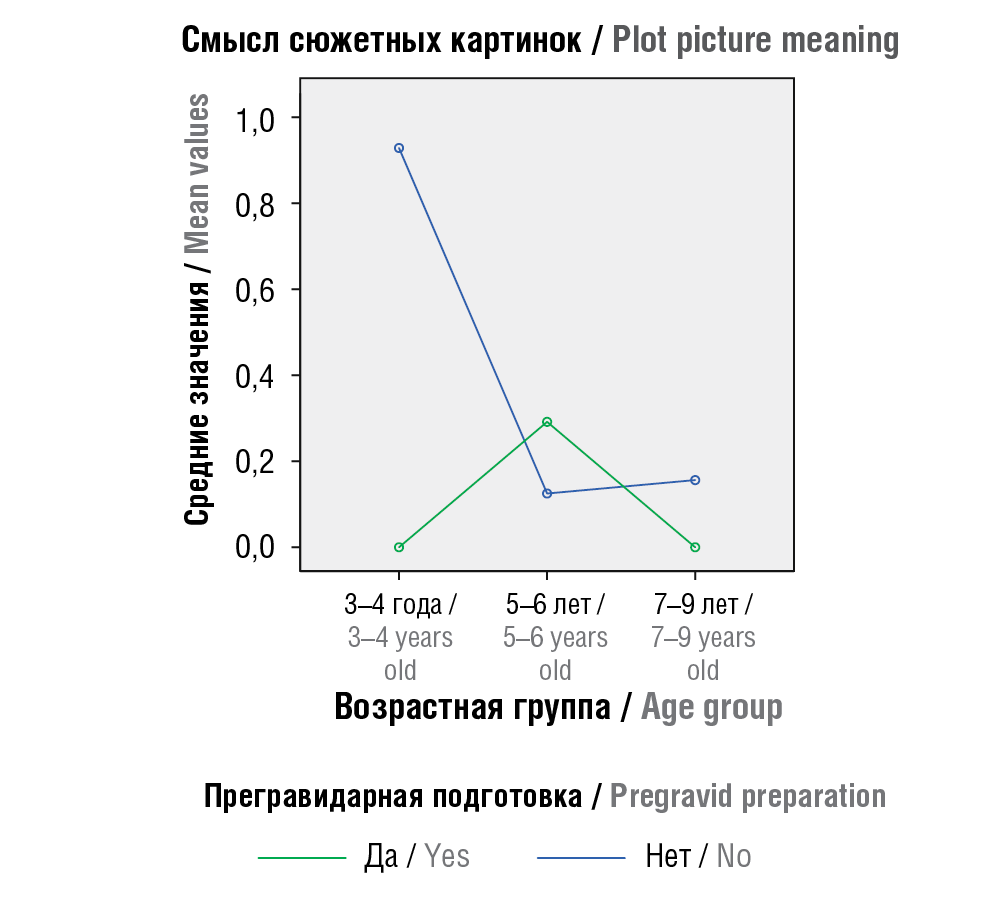
Figure 7. Level of understanding plot picture meaning in children depending on pregravid preparation for mothers with epilepsy
Рисунок 7. Уровень понимания смысла сюжетных картинок у детей в зависимости от проведения матерям с эпилепсией прегравидарной подготовки
Predictors of a child's mental development disorders / Предикторы нарушений психического развития ребенка
The regression analysis results revealed a number of disorder predictors for further child's mental development. Among all pregnancy complications, toxicosis of the first half along with pre-pregnancy seizures and lack of pregnancy preparation exerted most destructive effect. In such case, children showed the greatest number of problems in various areas of mental development (Fig. 8a). Conversely, conducting pregravid preparation in focal epilepsy, but not in the case of artificial feeding, are predictors for a child's potential to successfully cope with “Arithmetic” subtest requiring to concentrate arbitrary attention, ingenuity, and precise operation of numerical material (Fig. 8b).
Thus, pregnancy planning and pregravid preparation for mothers with epilepsy are crucial factors for preventing neurobehavioral teratogenesis, which lower risk of child’s disorders, thereby increasing its potential for mental development.
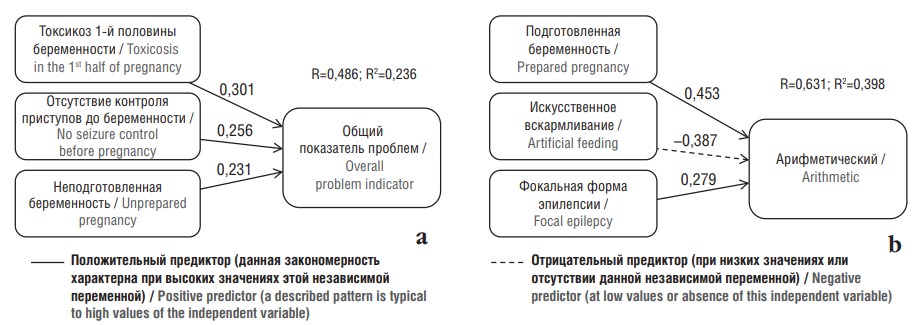
Figure 8. Predictors of mental development disorders in children born to mothers with epilepsy:
a – predictors of total number of developmental and adaptation problems; b – predictors of ability to operate with numerical material.
R – coefficient of multiple correlation; R2 – coefficient of multiple determination. Above the arrows, values of beta-coefficients are indicated demonstrating the “contribution” of this specific variable to overall regression
Рисунок 8. Предикторы нарушений психического развития у детей, рожденных матерями с эпилепсией:
а – предикторы общего количества проблем развития и адаптации; b – предикторы способности оперировать числовым материалом.
R – коэффициент множественной корреляции; R2 – коэффициент множественной детерминации. Над стрелками указаны значения бета-коэффициентов, которые демонстрирует «вклад» данной переменной в общую регрессию
Moderator analysis / Анализ модераторов
As a result of the moderators’ analysis, we also discovered that pregravid preparation was a moderator of epileptic seizures and pregnancy complications (toxicosis) in the mother on further mental development and adaptation of paired children. Eleven moderators were identified.
Seizures during pregnancy are a predictor of emergence of a large number of further child’s mental development disorders particularly somatic issues, attention disorders, motor awkwardness, externalization problems, including aggression (Fig. 9). Conducting pregravid preparation markedly lowers predictive power of this effect.
It was also found that toxicosis is a predictor for emerging further child’s externalization problems including aggression, delayed development of neurodynamics, orientation, adequacy and criticality in neuropsychological examination (Fig. 10), whereas conducting a pregravid preparation significantly reduces the predictive power of this effect.
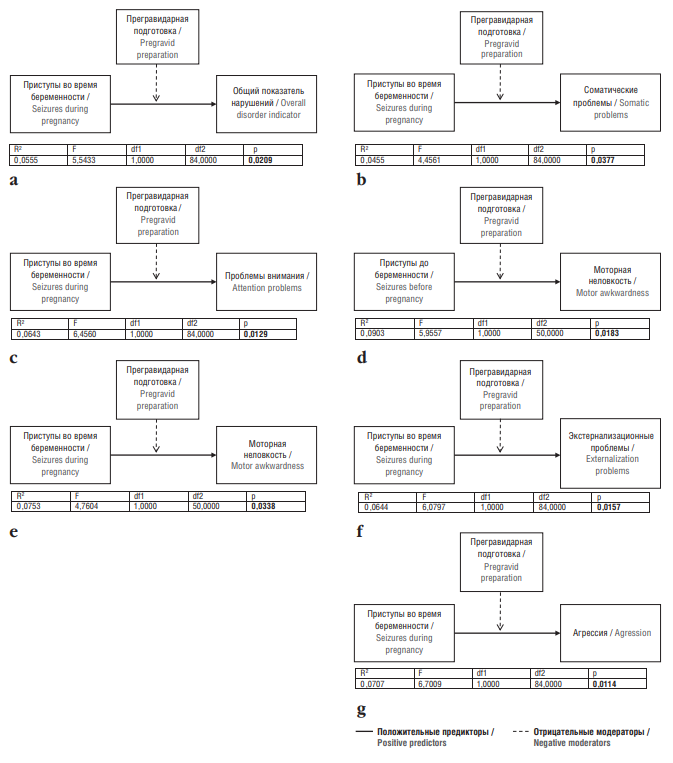
Figure 9. Moderators of maternal epileptic seizures impact on a child’s subsequent mental development and adaptation:
a – probability of mental development and adaptation disorders (moderator 1); b – probability of somatic problems (moderator 2); c – probability of attention disorder (moderator 3); d – probability of motor awkwardness due to seizures before pregnancy (moderator 4); e – probability of motor awkwardness due to seizures during pregnancy (moderator 5); f – probability of externalization problems (oppositional defiant disorder, delinquent behavior, aggression) (moderator 6); g – probability of aggression (moderator 7).
R2 – coefficient of multiple determination (what percentage of the sample is accounted for by independent variable); F – statistical criterion;
df1, df2 – degrees of freedom; p – significance level
Рисунок 9. Модераторы влияния эпилептических
приступов у матери на дальнейшее психическое развитие и адаптацию ребенка:
a – вероятность появления нарушений психического развития и адаптации (модератор 1); b – вероятность появления соматических проблем (модератор 2); c – вероятность нарушения внимания (модератор 3); d – вероятность возникновения моторной неловкости из-за приступов до беременности (модератор 4); e – вероятность возникновения моторной неловкости из-за приступов во время беременности (модератор 5); f – вероятность появления экстернализационных проблем (оппозиционно-вызывающее расстройство, делинквентное поведение, агрессивность) (модератор 6); g – вероятность появления
агрессии (модератор 7).
R2 – коэффициент множественной детерминации (какой процент выборки объясняется влиянием независимой переменной); F – статистический критерий; df1, df2 – степени свободы; p – уровень значимости
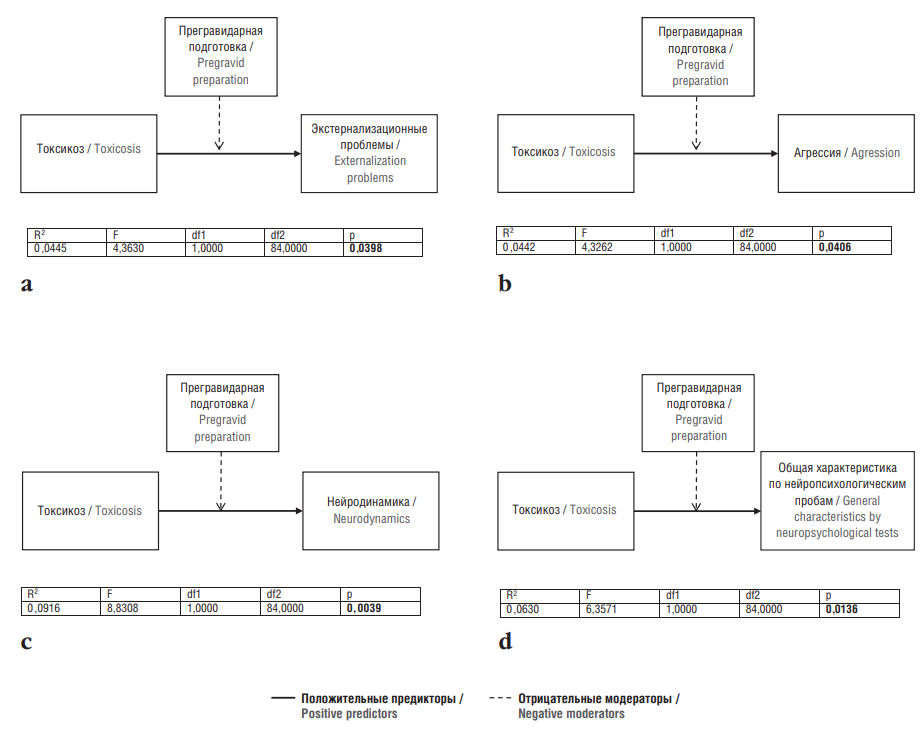
Figure 10. Moderators of maternal toxicosis impact on further child’s mental development and adaptation:
a – probability of externalization problems (moderator 8); b – probability of aggression (moderator 9); c – probability of delayed neurodynamics development (moderator 10); d – probability of manifestation of insufficient orientation, adequacy and criticality (moderator 11).
R2 – coefficient of multiple determination (what percentage of the sample is accounted for by independent variable); F – statistical criterion; df1, df2 – degrees of freedom; p – significance level
Рисунок 10. Модераторы влияния токсикоза у матери на дальнейшее психическое развитие и адаптацию ребенка:
a – вероятность появления экстернализационных проблем (модератор 8); b – вероятность появления агрессии (модератор 9); c – вероятность задержки развития нейродинамики (модератор 10); d – вероятность проявления недостаточной ориентировки, адекватности и критичности (модератор 11).
R2 – коэффициент множественной детерминации (какой процент выборки объясняется влиянием независимой переменной); F – статистический критерий; df1, df2 – степени свободы; p – уровень значимости
Relevance and prospects of research / Актуальность и перспективы исследований
The presented report assessed a role of pregravid preparation on child’s mental development due to the lack of data regarding neurobehavioral teratogenesis in children born to women with epilepsy. This type of studies is an interdisciplinary that accumulates efforts and integrates data from several groups of specialists – psychologists, neurologists and obstetricians-gynecologists, which is challenging. Despite being highly demanded and due to its practical significance for clinical practice, this research field is in infancy and has not yet fully achieved scientific potential [22].
The results of previous studies regarding mental and intellectual development in children born to mothers with epilepsy are very contradictory. It is worth mentioning that attention was primarily drawn to delayed psychomotor development, behavior problems in children who are exposed to various teratogenic factors in utero due to maternal epilepsy [23]. In the works conducted by Russian and foreign researchers, it was revealed that mothers with epilepsy who received old-generation AEDs were more likely to give birth to children with congenital malformations, e.g., spina bifida, hypospadias, congenital heart defects [24]. Unfortunately, the importance of publications on congenital malformations in maternal epilepsy still remains relevant [25].
Changes in AEDs spectrum used during pregravid preparation and pregnancy affected incidence of congenital malformations, the frequency and pattern of neurocognitive disorders in children born to mothers with epilepsy. According to the European Registry of Pregnancy in Epilepsy, the administration of lamotrigine dominates, whereas use of older-generation AEDs declines [2]. The usage of lamotrigine is associated with no negative effect on mental development in children born to mothers with epilepsy
A modern trend in the reproductology of epilepsy has become a strategy focused on average reproductive behavior. In the cohort, the average age of mothers at birth is 27 years old, with average epilepsy duration comprising 15 years. The predominance of epilepsy onset at puberty and the long disease length increase a risk of developing reproductive endocrine disorders and substantiate a need to study hormonal profile within pregravid preparation [9]. Taking into account the high frequency of endocrine infertility in epilepsy, assisted reproductive technologies have become more widely used. Thus, new directions are being created while assessing neuropsychological development in children born to mothers with epilepsy by using assisted reproductive technologies [26].
Pregravid obstetric and gynecological preparation reduces the incidence of complications during pregnancy as well as risks of fetal pathology. A positive factor in pregravid epileptological preparation is the predominance of pregnancy occurring during AED monotherapy. The commitment to undergoing pregravid preparation characterizes the current trends in obstetric and gynecological practice in Russia and worldwide. Pre-pregnancy counseling (with further PP) should be carried out for all women of reproductive age at any planned and unscheduled visit [1].
For women with epilepsy, careful preparation for motherhood is justified not only by generally accepted recommendations, but also by the need for epileptological pregravid preparation, taking into account disease features to give birth to healthy offspring.
CONCLUSION / ЗАКЛЮЧЕНИЕ
The results obtained by using several types of statistical analysis have convincingly proved the crucial role for pregravid preparation in lowering the risks of emergence and compensation for disorders of neuropsychiatric development and adaptation in children born to mothers with epilepsy.
Comprehensive pregravid preparation is a moderator: it reduces the negative impact of AEDs, epileptic seizures and toxicosis during pregnancy on further child’s neuropsychiatric development and adaptation as well as increases compensation potential due to such disorders. Monotherapy with modern AEDs, control of seizures before and during pregnancy as well as prevention of pregnancy complications reduce the risks of neurobehavioral teratogenicity in children born to women with epilepsy.
Altogether, pregnancy of women with epilepsy should be planned and prepared taking into account somatic, obstetric-gynecological and epileptological aspects.
1. The Achenbach questionnaire was translated and adapted by T.V. Kornilova, E.L.Grigorenko, S.D. Smirnov at Vygotsky National Research Center "DAR" (Moscow) and The Yale Child Study Center (New Haven, USA), version EG – 1-2.
2. Orientation is a parameter that reflects how correctly a child names his age, class, date and month of birth, address, first name and patronymic of the parents, place of residence at the moment, the current time of the year and the date of the examination.
3. Adequacy is a parameter that reflects how child can control his behavior and how it corresponds to the examination situation.
4. Criticality is a parameter that reflects how much a child is interested in the results of an examination and adult's assessments, treats his mistakes adequately, worries, tries to correct himself, and formulates problems at school and at home (from the age of 9).
5. Luria neuropsychological batteries (adapted by Glozman) are standardized for each age. A child whose development corresponds to the age norm should successfully cope with the test, i.e. the number of errors should be 0. Figures 4–7 show that this is far from the case: children in all age groups made mistakes, but by the age of 7–9, those whose mothers had undergone pregravidar preparation were better “aligned” in their mental development.
References
1. Pregravidar preparation. Clinical Protocol of the Interdisciplinary Association of Reproductive Medicine Specialists. Version 2.0. Available at: https://praesens.ru/files/2020/broshyury/Protokol_MARS.pdf (in Russ.) (accessed 25.05.2024).
2. Tomson T., Battino D., Bromley R., et al. Management of epilepsy in pregnancy: a report from the International League Against Epilepsy Task Force on Women and Pregnancy. Epileptic Disord. 2019; 21 (6): 497–517. https://doi.org/10.1684/epd.2019.1105.
3. Craig J.J., Scott S., Leach J.P. Epilepsy and pregnancy: identifying risks. Pract Neurol. 2022; 22 (2): 98–106. https://doi.org/10.1136/practneurol-2019-002304.
4. Karlov V.A. Epilepsy in children and adult women and men. 2nd ed. Moscow: Binom; 2019: 896 pp. (in Russ.).
5. Li Y., Meador K.J. Epilepsy and pregnancy. Continuum. 2022; 28 (1): 34–54. https://doi.org/10.1212/CON.0000000000001056.
6. Ivanova N.E., Odintsova G.V., Oleinik A.A., Shchetinina A.M. Pregnancy and epilepsy: focus on seizure frequency changes and obstetric complications. Progress in studies and lag in practice. Nevrologiya, neiropsikhiatriya, psikhosomatika / Neurology, Neuropsychiatry, Psychosomatics. 2020; 12 (6): 77–82 (in Russ.). https://doi.org/10.14412/2074-2711-2020-6-77-82.
7. EURAP. An International Antiepileptic Drugs and Pregnancy Registry. Interim Report – May 2022. Available at: https://www.dgfe.org/fileadmin/user_upload/Service/EURAP/EurapReport_May2022_Germany.pdf (in Russ.) (accessed 25.05.2024).
8. Meador K.J., Baker G.A., Browning N., et al. Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurol. 2013; 12 (3): 244–52. https://doi.org/10.1016/S1474-4422(12)70323-X.
9. MacEachern D.B., Mandle H.B., Herzog A.G. Infertility, impaired fecundity, and live birth/pregnancy ratio in women with epilepsy in the USA: findings of the Epilepsy Birth Control Registry. Epilepsia. 2019; 60 (9): 1993–8. https://doi.org/10.1111/epi.16312.
10. Banach R., Boskovic R., Einarson T., Koren G. Long-term developmental outcome of children of women with epilepsy, unexposed or exposed prenatally to antiepileptic drugs: a meta-analysis of cohort studies. Drug Saf. 2010; 33 (1): 73–9. https://doi.org/10.2165/11317640-000000000-00000.
11. Baranov A.A., Maslova O.I., Namazova-Baranova L.S. Ontogenesis of neurocognitive development of children and adolescents. Annals of the Russian Academy of Medical Sciences. 2012; 67 (8): 26–33 (in Russ.). https://doi.org/10.15690/vramn.v67i8.346.
12. Wiedemann K., Stüber T., Rehn M., Frieauff E. Fetal valproatesyndrome – still a problemtoday! Z Geburtshilfe Neonatol. 2017; 221 (5): 243–6. https://doi.org/10.1055/s-0043-107619.
13. Razaz N., Tomson T., Wikström A.K., Cnattingius S. Association between pregnancy and perinatal outcomes among women with epilepsy. JAMA Neurol. 2017; 74 (8): 983–91. https://doi.org/10.1001/jamaneurol.2017.1310.
14. Meador K.J., Cohen M.J., Loring D.W., et al. Two-year-old cognitive outcomes in children of pregnant women with epilepsy in the maternal outcomes and neurodevelopmental effects of antiepileptic drugs study. JAMA Neurol. 2021; 78 (8): 927–36. https://doi.org/10.1001/jamaneurol.2021.1583.
15. Avakyan G.N., Blinov D.V., Lebedeva A.V., et al. ILAE classification of the epilepsies: the 2017 revision and update. Epilepsia i paroksizmal'nye sostoania / Epilepsy and Paroxysmal Conditions. 2017; 9 (1): 6–25 (in Russ.). https://doi.org/10.17749/2077-8333.2017.9.1.006-025.
16. Ustinovich A.A., Tkachenko A.K., Loginova I.A. Premature new born children: an educational and methodological guide. Minsk: BGMU; 2021: 36 pp. (in Russ.).
17. Blüml S., Wisnowski J.L., Nelson M.D. Jr., et al. Metabolic maturation of white matter is altered in preterm infants. PloS One. 2014; 9 (1): e85829. https://doi.org/10.1371/journal.pone.0085829.
18. Bakushkina N.I., Isaeva E.R. Longitudinal research of the dynamics of neurocognitive development in preterm and full-term infants from 5 to 24 months. Bulletin of Psychotherapy. 2022; 81: 40–9 (in Russ.). https://doi.org/10.25016/2782-652X-2022-0-81-40-49.
19. Kapellou O., Counsell S.J., Kennea N. Abnormal cortical development after premature birth shown by altered allometric scaling of brain growth. PLoS Med. 2006; 3 (8): e265. https://doi.org/10.1371/journal.pmed.0030265.
20. Tau G.Z., Peterson B.S. Normal development of brain circuits. Neuropsychopharmacology. 2010; 35 (1): 147–68. https://doi.org/10.1038/npp.2009.115.
21. Webb S.J., Monk C.S., Nelson C.A. Mechanisms of postnatal neurobiological development: implications for human development. Dev Neuropsychol. 2001; 19 (2): 147–71. https://doi.org/10.1207/S15326942DN1902_2.
22. Adab N., Kini U., Vinten J., et al. The longer term outcome of children born to mothers with epilepsy. J Neurol Neurosurg Psychiatry. 2004; 75 (11): 1575–83. https://doi.org/10.1136/jnnp.2003.029132.
23. Christensen J., Grønborg T.K., Sørensen M.J., et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA. 2013; 309 (16): 1696–703. https://doi.org/10.1001/jama.2013.2270.
24. Veroniki A.A., Rios P., Cogo E., et al. Comparative safety of antiepileptic drugs for neurological development in children exposed during pregnancy and breast feeding: a systematic review and network meta-analysis. BMJ Open. 2017; 7 (7): e017248. https://doi.org/10.1136/bmjopen-2017-017248.
25. Sivarajah K., Relph S., Sabaratnam R., Bakalis S. Spina bifida in pregnancy: a review of the evidence for preconception, antenatal, intrapartum and postpartum care. Obstet Med. 2019; 12 (1): 14–21. https://doi.org/10.1177/1753495X18769221.
26. Gorelova I.V., Chugunova A.A., Odintsova G.V. Epilepsy and assisted reproductive technologies: case report and literature review. Problemy reproduktsii / Russian Journal of Human Reprotuction. 2019; 25 (3): 57–62 (in Russ.). https://doi.org/10.17116/repro20192503157.
About the Authors
A. S. KraskoRussian Federation
Anastasia S. Krasko.
7-9 Universitetskaya Emb., Saint Petersburg, 199034
N. F. Mikhailova
Russian Federation
Nadezhda F. Mikhailova – PhD.
7-9 Universitetskaya Emb., Saint Petersburg, 199034
I. V. Larina
Russian Federation
Irina V. Larina.
9 lit. A Obvodnoy Channel Emb., Saint Petersburg, 192029
V. A. Mikhailov
Russian Federation
Vladimir A. Mikhailov - Dr. Sci. Med.
3 Bekhterev Str., Saint Petersburg, 192019
WoS ResearcherID B-3272-2017
G. V. Odintsova
Russian Federation
Galina V. Odintsova – PhD.
12 Mayakovskiy Str., Saint Petersburg, 191014
WoS ResearcherID G-8940-2012, Scopus Author ID 55510371000
Review
For citations:
Krasko A.S., Mikhailova N.F., Larina I.V., Mikhailov V.A., Odintsova G.V. “Between Scylla and Charybdis”: the influence of pregravid preparation on mental development of children born to mothers with epilepsy. Epilepsy and paroxysmal conditions. 2024;16(4):298-315. https://doi.org/10.17749/2077-8333/epi.par.con.2024.191
JATS XML

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.










































